Procedure Step Detection… On Steroids
![]() Theator
on
June 10, 2024
Theator
on
June 10, 2024
Can we skip to the good part?
Have you ever recorded an entire concert with your phone? Or a fireworks show? No one goes back to look at the whole thing, you want to fast-forward to the meaningful moments. Fast-forward to your favorite part or when something interesting happens.
It’s the same with surgery. Surgeons don’t have the time to go back and review hours of surgery after scrubbing out from a long day in the operating room.
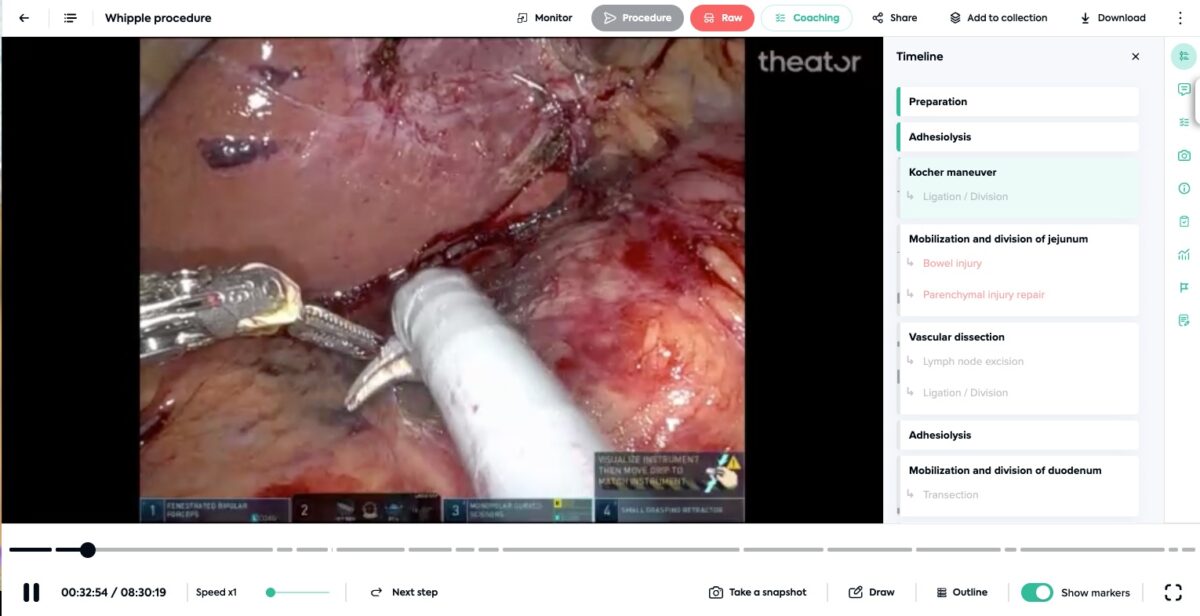
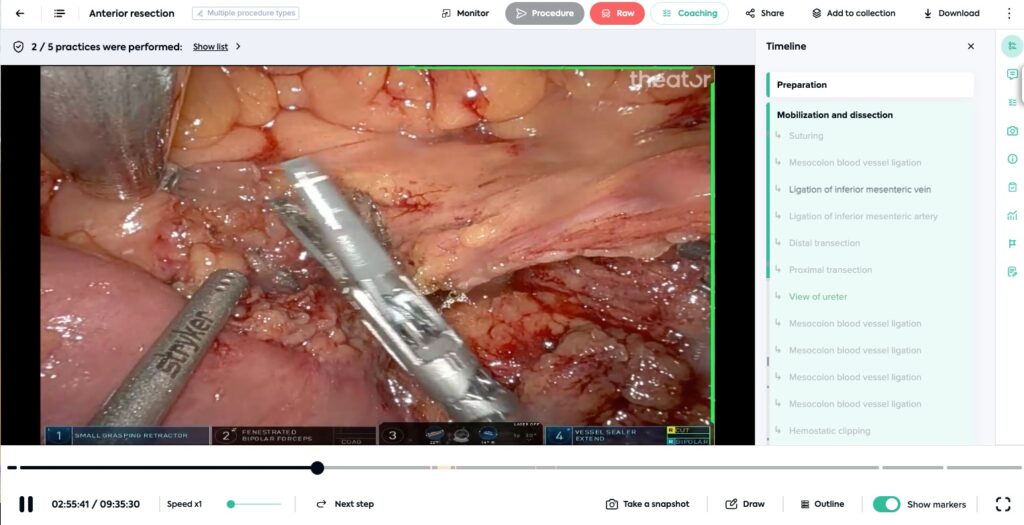
The two longest surgical videos in our database are (hours:minutes:seconds):
- Robotic anterior resection: 9:52:28
- Robotic whipple: 8:30:19
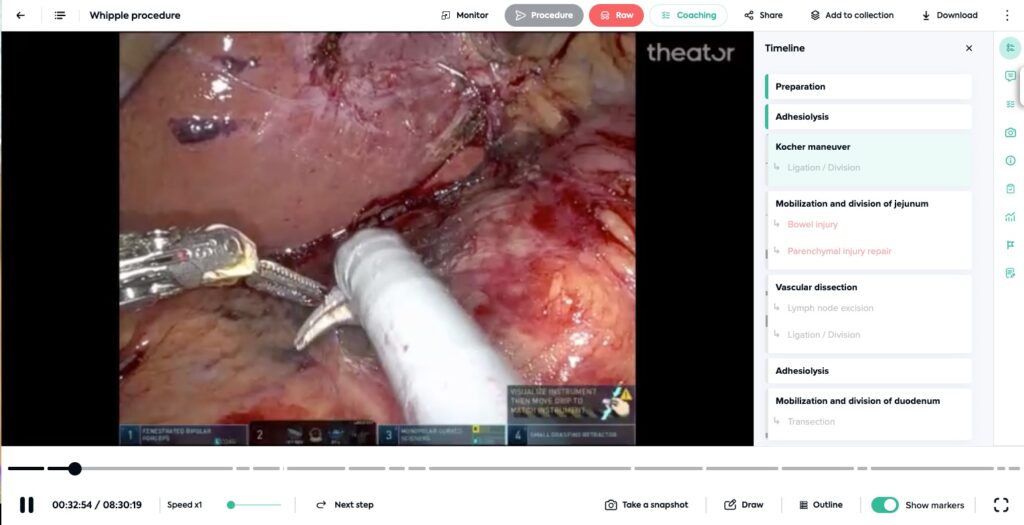
Even procedures this long, are automatically structured. With more than 3,000 procedures captured by Theator every week at a median duration of 42 minutes, that is a lot of data. A lot.
The video is yours, we just make sense of it
Surgical videos need to be structured to be useful. Not just with tools and time, but with all procedure steps, intraoperative events, surgical practices, and more. Structuring with procedure steps is the first step to extracting value from surgical video capture. A deep tech stack enables this to be possible and importantly, enables scalability.
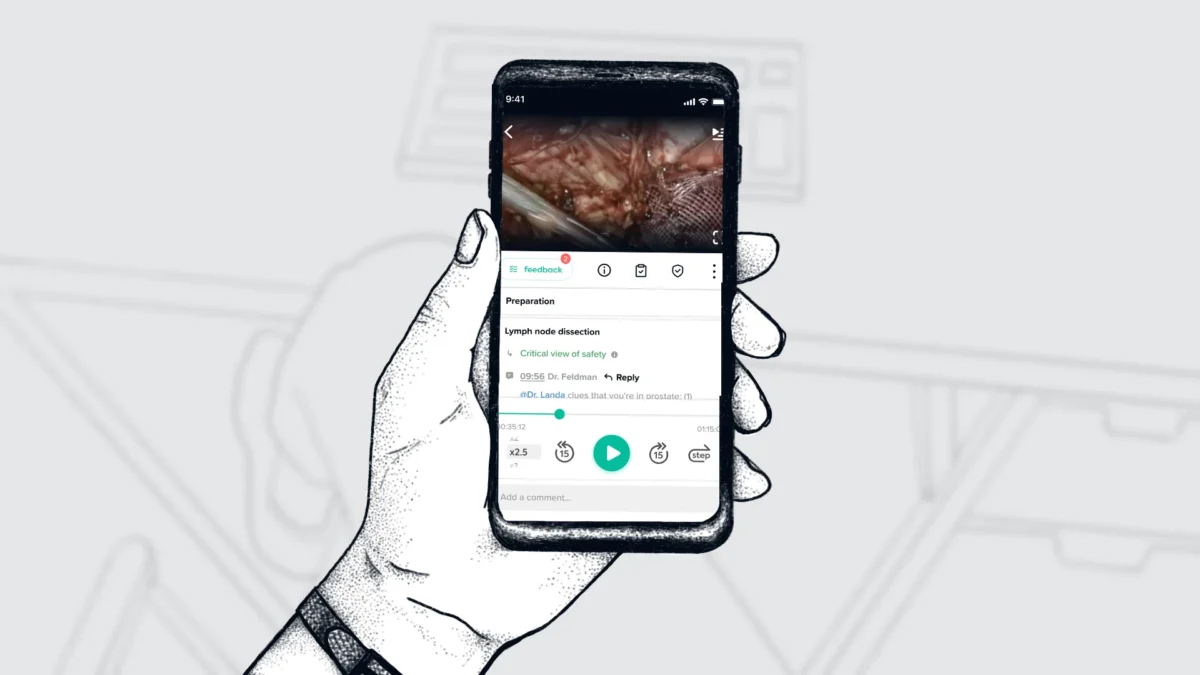
When a procedure is structured, surgeons can easily navigate to meaningful moments, trainees can quickly review interesting clips, surgical teams can quickly get answers to questions (read how one hospital confirmed no foreign body was left in a patient using quick video review), and so much more.
But, don’t just take it from us. A few abstracts and publications examples, written by our customers, have shown the ability of our AI tech to automate procedure step annotations (which, is just one element we structure). Check them out for yourselves below:
Urology
- Transurethral Bladder Tumor Resection (TURBT) – Frontiers in Artificial Intelligence
- Robotic-Assisted Radical Prostatectomy (RARP) – Journal of Urology
- Partial and Radical Nephrectomy – Society of Urologic Oncology
Gynecology
- Hysterectomy – published in the International Journal of Gynecology and Obstetrics
General Surgery
- Totally Extraperitoneal Inguinal Hernia Repair (TEP) – Surgical Endoscopy
Want to check these out all in one place? Download the cheat sheet here.