Improving The Modern Surgical Outcomes Report
In recent decades as evidence-based medicine became the standard of care, physicians and hospital systems turned to outcomes reporting as a means of indirectly measuring quality of care. Such information, especially when it is publicly available, allows for the transparency necessary to assuage patient concerns about the quality and safety of medical care and provides a basis for identifying systemic and individual opportunities for improvement.
No other area of medicine lends itself to outcomes reporting and tracking quite as well as surgery. The universal nature of surgical procedures allows for standardization of outcome metrics, and the inability of patients to provide an account of surgical occurrences reinforces the need for maximal transparency to monitor quality.
While outcomes reporting plays an undeniable role in improving care, as we enter the era of surgical AI augmentation, the time has come to ask ourselves whether outcomes reporting is enough. With so much data now at our fingertips, how can it be harnessed to increase transparency and further improve outcomes?
The Actual Impact of Reporting Surgical Outcomes
The use case for surgical outcomes reporting came from cardiothoracic surgeons in the UK. This formal reporting process was born out of public pressure related to high mortality rates of pediatric patients in the region undergoing cardiothoracic surgery. With all pediatric cardiac units required to participate in outcomes reporting, mortality decreased 75% between 1985 and 2002.
Following this, the Society for Cardiothoracic Surgery in Great Britain and Ireland began publishing hospital- and physician-specific data in 2005, resulting in a 50% reduction in risk-adjusted mortality. Since 2005, seven additional surgical specialties in the UK started publishing their outcomes data.
This practice has a number of advantages, most especially for patients for whom the transparency of outcomes reports provides trust and autonomy in their healthcare decision making. Surgeons also benefit from outcomes tracking, which allows identification of hospitals and surgeons with the best outcomes who can, in turn, inform best surgical practices. Additionally, publishing outcomes data provides a transparent piece of the complex puzzle that is healthcare costs.
Surgical Outcome Reports Don't Tell The Whole Story
Without an automated means of capturing outcomes data, continued dependence on human reporting will be inherently suboptimal due to incomplete recall and documentation.
Related to this is the fact that outcomes alone do not take into account patient-specific pre-surgical risk and other factors that affect the complexity of a case. In other words, the intraoperative death of an 85-year-old patient with multiple comorbidities is clinically different from that of a 25-year-old previously healthy patient undergoing the same procedure. While some outcomes reporting systems attempt to account for this risk difference with adjusted scores, there is no perfect way of representing these factors.
In addition, outcomes reports are inherently inaccurate to a certain extent due to their dependence on retrospective reporting. One study found that routine reporting by surgeons identified only 62% of adverse outcomes and even medical chart review identified only 78%.
Without an automated means of capturing outcomes data, continued dependence on human reporting will be inherently suboptimal due to incomplete recall and documentation.
How Do We Go Beyond Surgical Outcomes Reporting?
Outcomes reporting provides an important level of professional and public transparency that can build patient trust and potentially result in practice improvement. However, the latter is not a guaranteed result of outcomes reporting alone. One study that compared 263 hospitals that participated in The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) to 526 that did not found no statistically significant improvement in outcomes across a 3-year period at participating hospitals, leading the authors to conclude that feedback on outcomes alone is not enough to prompt improvement.
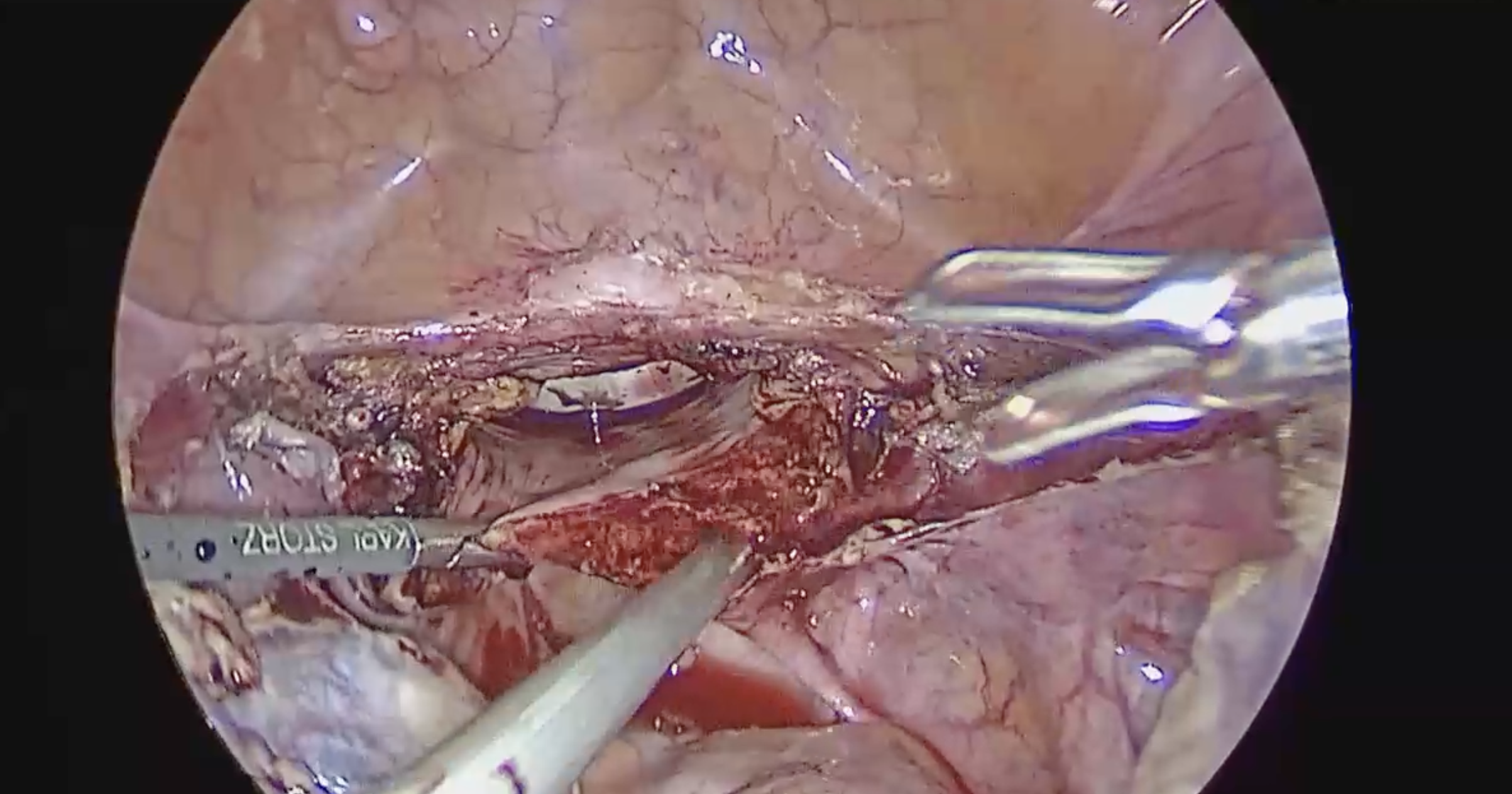
For outcomes to serve as meaningful tools for improvement, they must be associated with additional information that tells the story behind how and why an outcome occurred. For surgeons, this data lies mainly in the events that occur in the OR during a surgical procedure. Intraoperative video recording offers a goldmine of data that, when paired with information about surgical outcomes, can provide the key to translating these outcomes into improved surgical practices.
The concept of recording all surgical procedures as standard practice has understandably been met with trepidation by some surgeons. After all, as Alexander Langerman, MD states, “no one wants to fall below the bell curve.” This, coupled with the litigious nature of today’s healthcare system, can lead surgeons to disproportionately focus on the risks of transparency while disregarding the benefits.
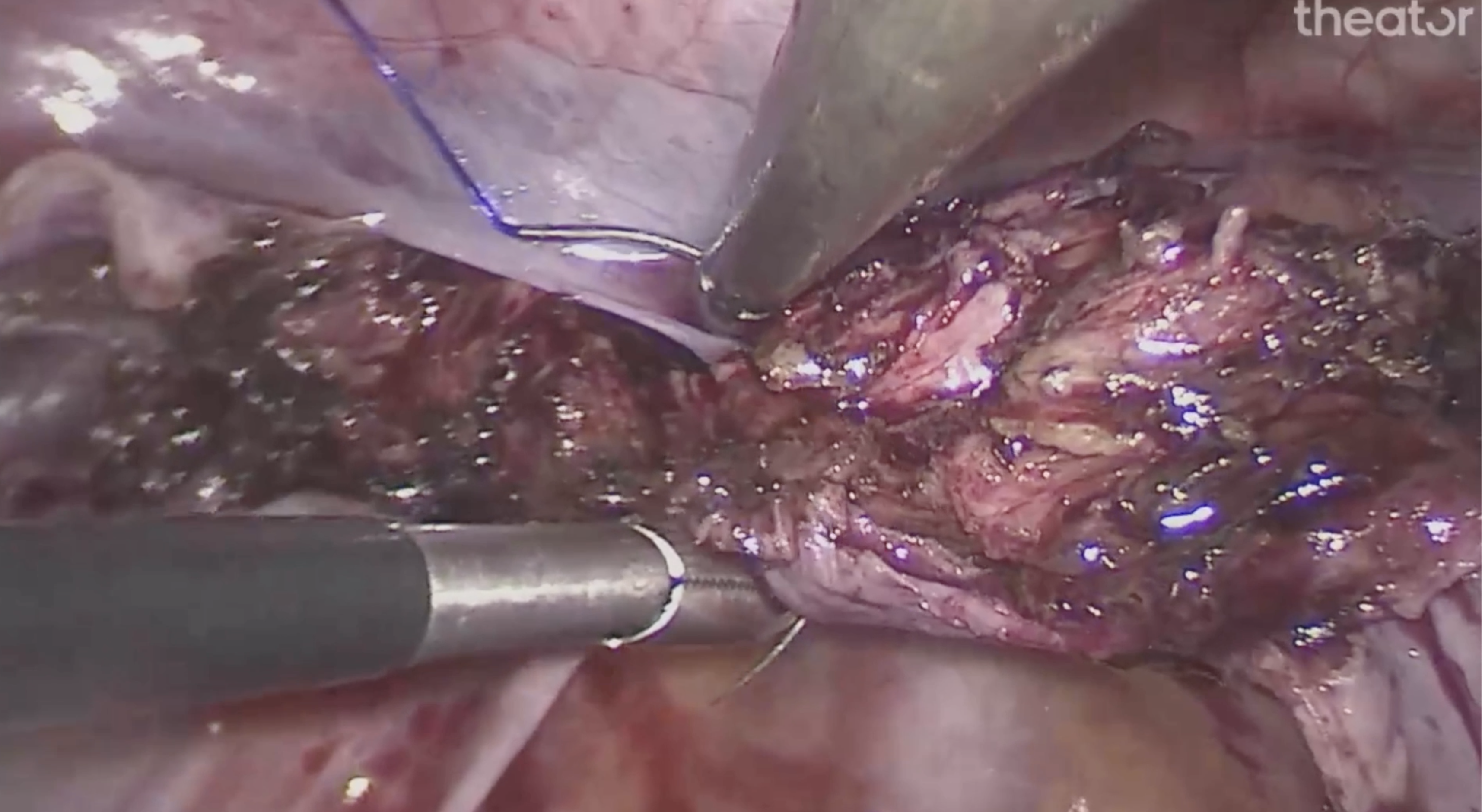
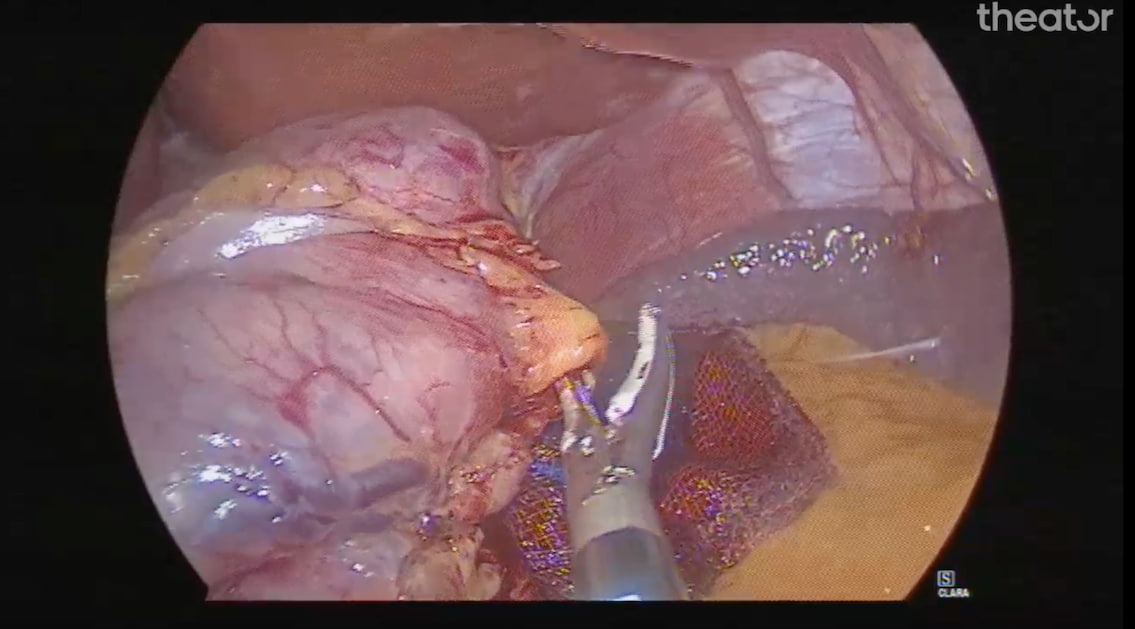
However, the benefits of intraoperative video analysis are well documented. For example, one study that used AI to analyze hundreds of intraoperative hysterectomy videos in search of practice differences to explain variability in outcomes found that not all surgeons were performing the recommended step of identifying the ureters during the procedure. This critical part of a hysterectomy procedure is key to preventing ureter injuries, and yet it was not being consistently performed.
This is only one example of how AI analysis of intraoperative video can serve as an essential component of the quality improvement process. AI offers the ability to review and analyze surgical video in a manner that is impossible for surgeons to do manually due to time constraints. Without this tool and the transparency it offers, the reasons behind variability in surgical outcomes cannot be easily identified, and the practice modifications needed to improve these outcomes will remain a mystery.
Taking Surgical Transparency to the Next Level
Digital tools, including AI technologies that analyze intraoperative surgical video, are no longer the wave of the future. Instead, they are already present in ORs and being used by surgeons who see the value they offer in increasing transparency, identifying practice variability, and improving outcomes. The takeaway in the dawning of this new era in which medical care and technology are more intertwined than ever is that increasing transparency by embracing these tools will be a defining characteristic of surgeons who strive to continuously improve, and those who do not embrace these technologies will be left behind.