The impacts of surgical variability extends far beyond individual procedures
Simply put, “surgical variability” means not all surgeons perform surgery exactly the same way. Because of the many factors contributing to variability between procedures, reducing variability is a challenge hospital administrators are painfully aware of. Some causations are obvious, like patient factors or healthcare inequity. While others are more opaque—like subjective experiences between surgeons, or a lack of actionable data.
The effects of surgical variability at every level of the healthcare ecosystem are significant and wide-ranging. It’s no wonder that executives, administrators, and surgical teams have long been in search of reliable ways to reduce or eliminate it altogether.
Variability in surgical care often leads to preventable complications and poor outcomes, but patients are not the only ones feeling the negative impacts of surgical variability…
To patients surgical variability can mean life or death
Obviously the group hardest hit by disparities in surgical care is patients. The worst case scenario for them, of course, is preventable death. But even unforeseen complications resulting in longer hospital stays, additional health issues, or the need for reoperation can take a massive toll. Patients miss work, incur huge hospital bills, have their lives interrupted, endure pain, discomfort, and lack of privacy, and often suffer psychological distress due to these experiences.
The burden of variability also weighs heavy on caregivers & loved ones
Those closest to the patient experience the ripple effects of the events described above. From managing and coping with the death of their loved one to providing assistance that also disrupts their daily lives and drains them of time, money, energy, and mental health, entire communities feel the impact of surgical variability.
The psychological impact of variability on surgeons
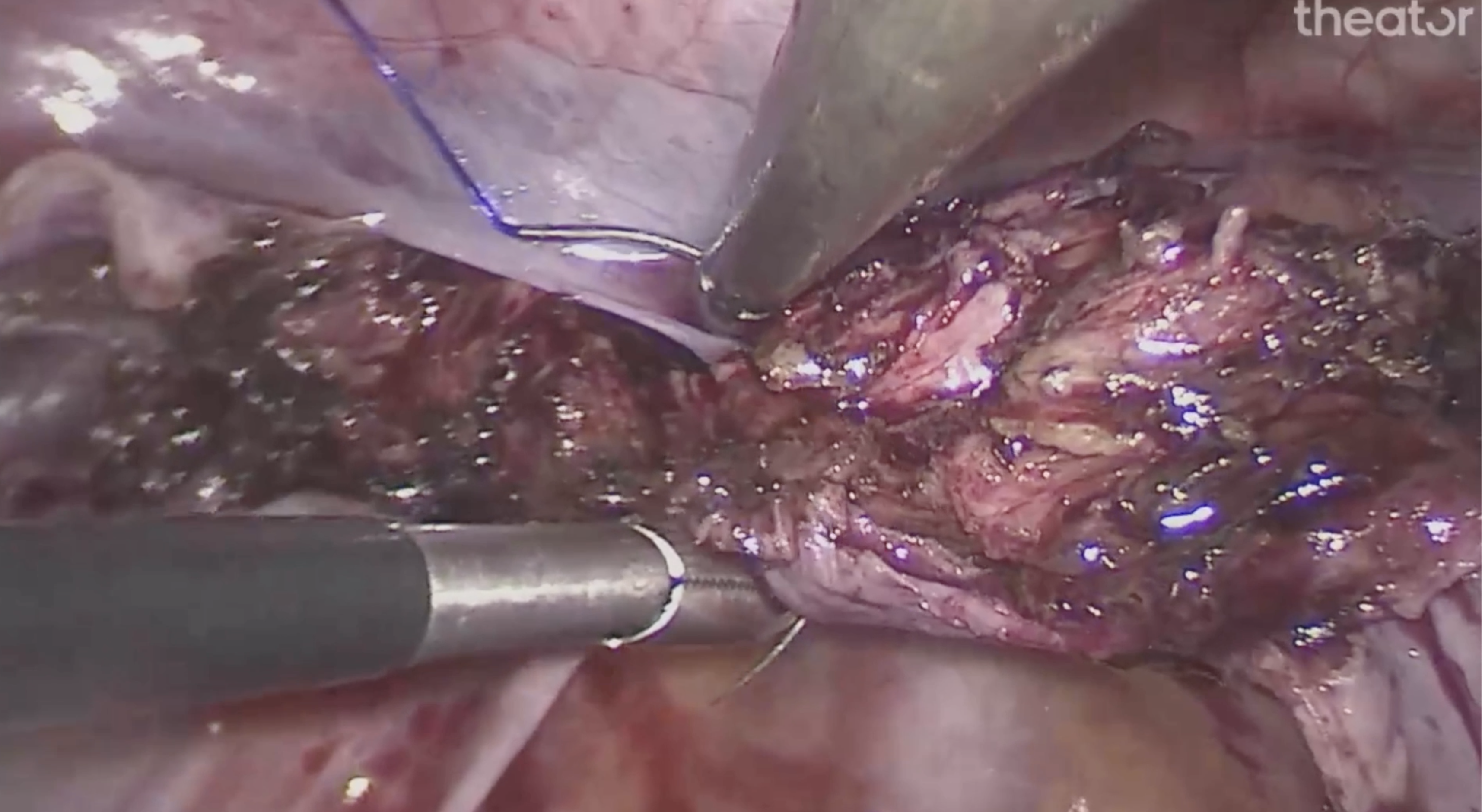
Generally speaking, surgeons and surgical staff strive to continuously hone their craft and deliver the best possible outcomes for their patients. But pervasive variability in processes and techniques (and especially the visibility issues that cause that problem) limits their ability to develop professionally — and to help others improve. The resulting complications and negative outcomes also take a psychological toll on them.
The financial, operational, and liability implications of variability on hospitals
The financial and operational impact on individual hospitals is tremendous. Estimated costs incurred due to gastric leak in laparoscopic sleeve gastrectomy are up to $10,000 per incident — and that’s just one complication that occurs in one type of procedure in one specialty. Hospitals also have to contend with liability issues, such as malpractice suits, insurance reimbursement, and more. And operationally speaking, even what may seem like minor efficiency issues, when replicated across thousands of procedures per year, can add up in terms of budget, resources, and patient care. In a system already stretched too thin, these institutions can ill afford the effects of surgical variability.
Health systems carry the consequences of variability at scale
Similar to how the impact on patients ripples outward to their communities, the impact on hospitals ripples throughout health systems, eating up precious resources that could be used to improve care. No one can “afford” to fix the problem, but the problem itself is costing an ever-growing fortune.
Surgical Variability: A problem we can’t afford to ignore.
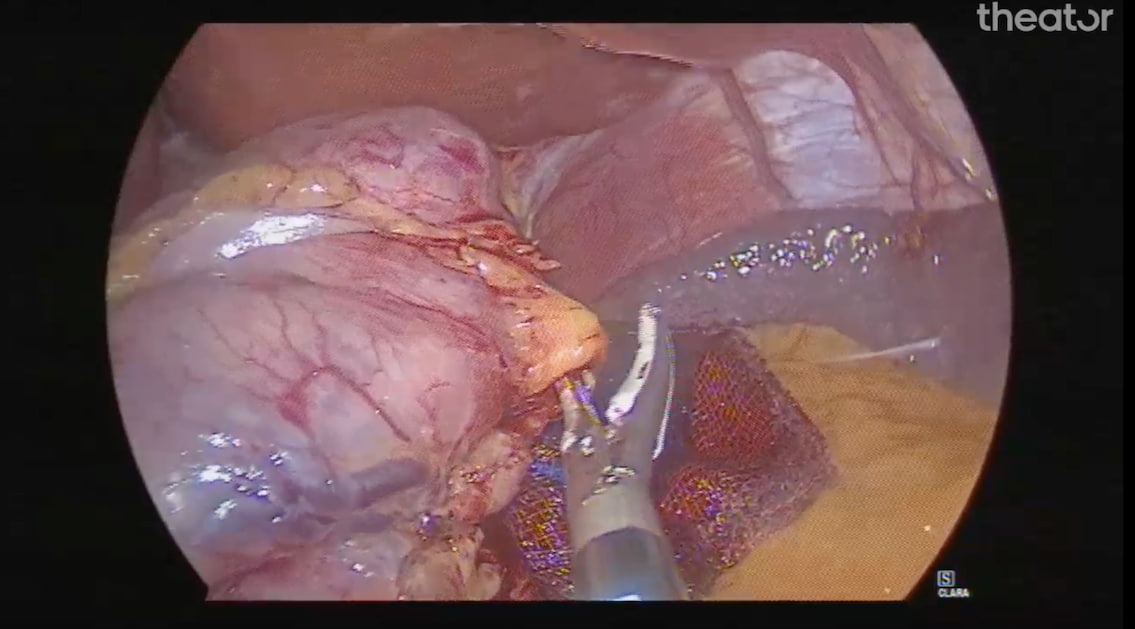
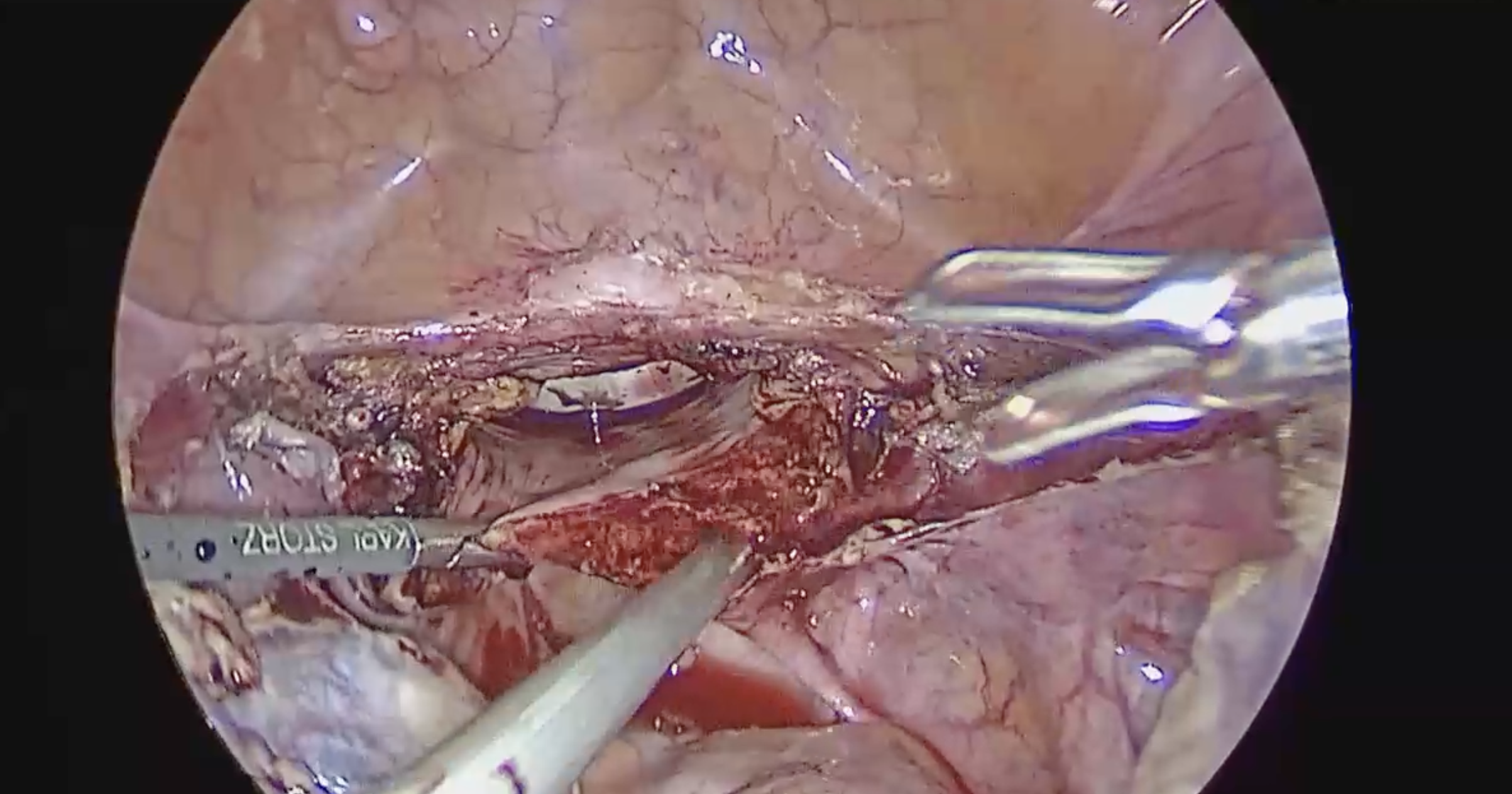
Surgical variability has significant implications on the entire healthcare ecosystem, it’s clear that this is an issue we cannot afford to ignore. Though it’s unlikely that we can eliminate this issue entirely, there are steps we can take today to reduce avoidable procedural variability by driving standardization in adoption to evidence-based, surgical best practices. Only by capturing, structuring, and analyzing surgical data, we can surface intraoperative variability that impacts postoperative recovery and start to solve variability one department at a time.
Ready to start reducing variability?
Download our Beginners Guide to Surgical Variability eBook: