The Frequency of Surgical Complications is Alarmingly High
From the earliest days of trepanation to modern minimally invasive techniques, we’ve come a long way in the field of surgery. But we’re still far from perfect. In fact, of the 300 million surgical procedures performed annually, nearly 1 in 6 still involve complications, resulting in around 3 million deaths per year. The subsequent physical, emotional, and psychological effects on patients and their loved ones, as well as the massive financial and operational impact on hospitals and surgical teams, are impossible to overstate.
The Role of Surgical Variability in Complication Prevention
Variability in surgical care contributes to this high incidence of preventable complications and poor outcomes, and stems from a lack of adoption to data-driven surgical practices. And disparities aren’t limited to less-developed regions. We see variability between hospitals — and even departments — in major metropolitan centers of the most developed countries on Earth.
Administrators are painfully aware of this challenge, but have struggled to find any reliable way of solving it. Many hospitals invest heavily in hiring teams to analyze their own data and/or to participate in The American College of Surgeons National Surgical Quality Improvement Program (NSQIP). While the program is designed to measure and improve the quality of surgical care, participation does little more than confirm variability exists and show how participants measure up against their peer hospital groups.
You don’t need sample data that’s delayed 6 months (and isn’t actionable) to tell you any of that. You need better ways to understand why this surgical variability exists in the first place, pinpoint specific areas of improvement, set goals, and achieve them. But let’s start with surgical variability: its causes, effects — and what hospitals and surgical teams can start doing about it now.
What causes surgical variability?
In its most literal sense, “surgical variability” means “not all surgeons perform surgery exactly the same way.” When we break down any procedure into its component steps (assuming even these are standardized), there are any number of different circumstances that could arise, techniques that could be employed, or processes that could be followed during each step that influences the outcome.
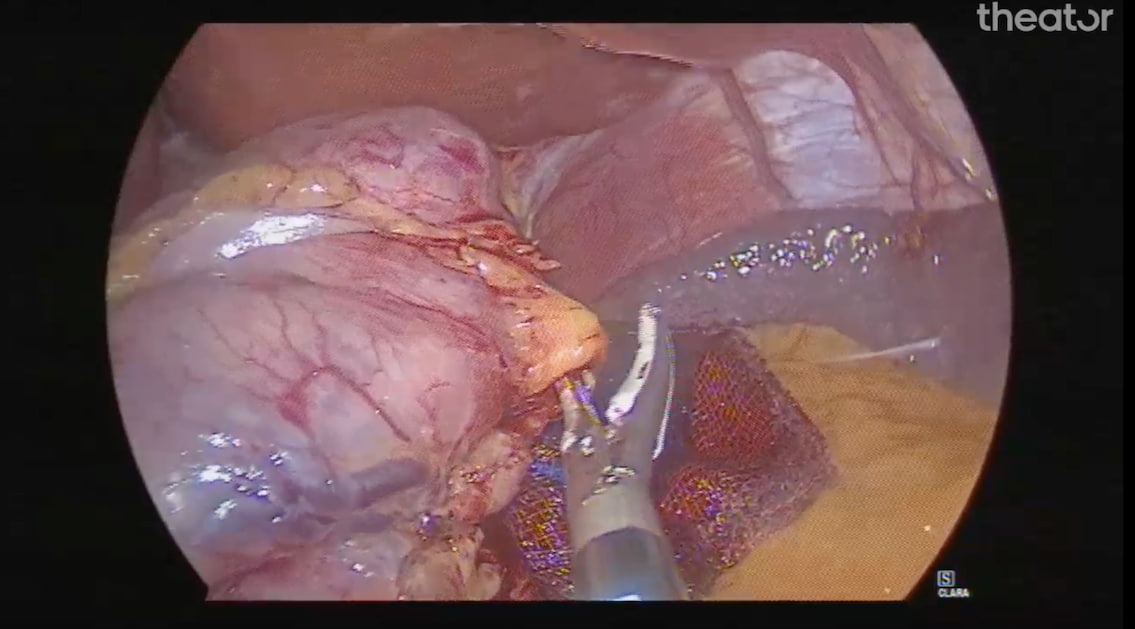
For example, during a laparoscopic sleeve gastrectomy, oversewing the staple line has been shown to help prevent gastric leak and bleeding — two of the most serious complications of this common procedure. Yet a recent analysis of 370 sleeve gastrectomies revealed this technique was performed in only 60% of cases.*
The same analysis also revealed significant variability in surgical efficiency, with average time to perform a specific step, the gastric transection, as low as 13 minutes and 20 seconds for some surgeons, and nearly 39 minutes for others. Considering that longer procedure times are associated with poorer patient outcomes and higher hospital costs, this is no small matter.
While all these opportunities for deviation might seem to create an infinite number of un-trackable variations, there are some common threads that can help us make sense of it all:
- Healthcare inequity. Unfortunately, socioeconomic factors, inherent bias, and other equality-based considerations often cause disparities in care and outcomes. From limited access to even basic care (let alone advanced technologies) to communication and trust issues, myriad factors put a disproportionate share of the negative effects of surgical variability on historically marginalized populations.
- Patient factors. Every patient is different. Some have pre-existing conditions that put them at higher risk during certain procedures or specific techniques. Some have anatomical anomalies that require in-the-moment adjustments or deviations from standard practices. But particularly with common procedures that are performed thousands of times every day across the world, we should be able to account for these factors by now with documented surgical practices.
- Subjective experience. Due to the age-old apprenticeship model of surgical training, one surgeon’s career-long experience can be dramatically different from another’s without either ever realizing it. When your training and daily practice are so heavily guided by the subjective experience of one person (who learned many of the same things, the same way, from yet another single person, and so on), your perspective is inherently narrow and biased.
- Lack of actionable data. Although many aspects of surgery are tracked and reported, surgical teams often suffer from “DRIP” (data-rich, insight-poor) visibility issues. Sometimes there’s a scarcity of proof to back up new or emerging recommendations, making surgeons more hesitant to adopt them. And sometimes the data that could be most helpful is simply not reliable or accessible. For example, the best record most hospitals currently have of what goes on in the OR is the surgeon’s operative report. These are typically templatized, created after the fact, and (as has been widely reported) often highly inaccurate. In fact, one paper, entitled A Video is Worth a Thousand Operative Notes revealed that while operative reports claimed 85.1% of technical steps were followed, operative video confirmed only 52.5% actually had been.
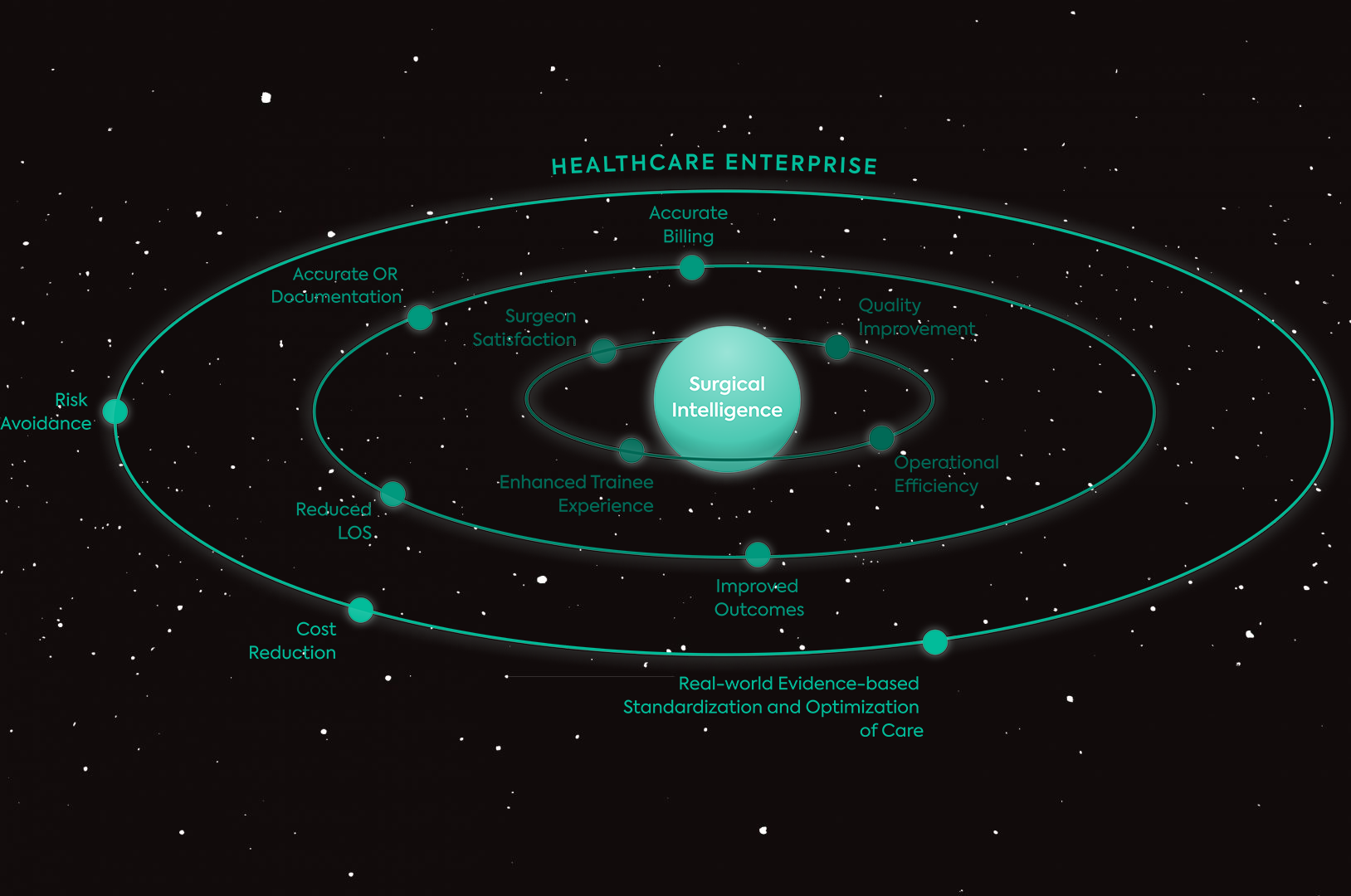
Surgical Intelligence: The Next Step to Reducing Variability
Because of these factors, completely eliminating surgical variability may not be possible. But we have the resources to start reducing variability by a significant margin. Powered by AI and machine learning, Surgical Intelligence can help us connect the dots between patient characteristics, surgical practices, and post-op results. Because it’s understanding surgical outcomes is not enough, we have to understand how specific decisions and practices impact those outcomes.
Ready to start reducing variability?
Download our Beginners Guide to Surgical Variability eBook:
*References: Theator Surgical Intelligence Platform Data on File: Bariatric Procedure Analysis, 2023.
Dobson GP. Trauma of major surgery: A global problem that is not going away. Int J Surg. 2020 Sep;81:47-54. doi: 10.1016/j.ijsu.2020.07.017. Epub 2020 Jul 29. PMID: 32738546; PMCID: PMC7388795.