What does AI have to do with the operating room?
Multiple innovations have struck the surgical world. These technologies offer an eclipse into the future of surgery, each attempting to revolutionize the way operations are performed today. In the past, surgical innovation spurred around medical devices: a better stapler, more advanced monitoring equipment, or a versatile surgical robot. All these advancements are hardware.
While these devices start to mature, there has been a clear shift toward software-based innovations. The new buzzword is Artificial Intelligence. So what is AI, and how is it related to the OR?
The Oxford dictionary defines AI as: “the theory and development of computer systems able to perform tasks that require human intelligence, such as visual perception, speech recognition, and translation between languages.”
It is clear that technology for the sake of technology is useless; therefore, it is imperative to determine the pain points these innovations attempt to address. AI alone is merely a technological advancement; the question is what value it brings to the table.
Until now, surgical software companies have been divided into four categories:
#1: Telesurgery
The world went virtual as the covid-19 pandemic erupted. Employees began working remotely, and many technologies were developed to enable efficient work from afar. If remote video calls can substitute presence in a conference room, why can’t they replace physical presence in the operating room? Companies in this space are essentially creating zoom or facetime for the OR. Despite being a novel technological solution, this platform doesn’t use artificial intelligence. While telesurgery may help to improve access to surgical care, it’s unscalable. Telesurgery is a one-to-one solution that relies on subjective surgeon experience and surgical experts’ availability when needed.
#2: Enhanced Visualization
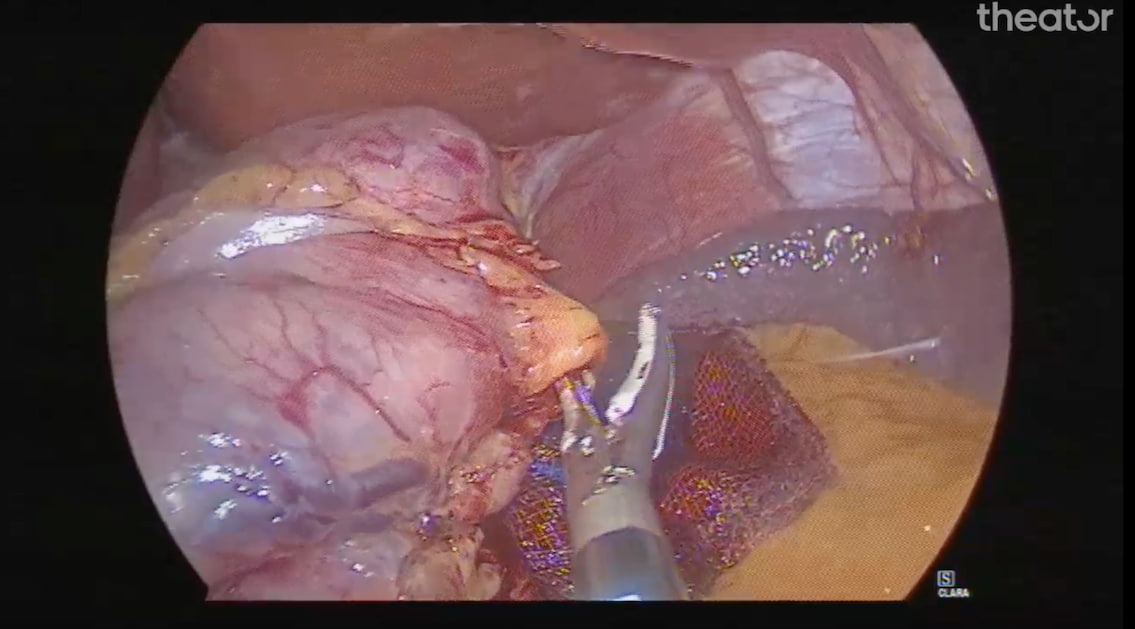
Innovations within this category are developing anatomical enhancement systems that improve visualization of the operative field.
While these solutions may make it easier to perform the next step in surgery, they do not necessarily inform what that step should be or how it should be performed. They address a specific element of surgery but not surgical practice as a whole and therefore don’t address surgical variability.
#3: OR Performance Monitoring
Surgical treatment is a sophisticated process and, therefore, vulnerable to human error. Periodically, news reports cases where surgery was performed on the wrong body part. Surgical safety is a well-documented issue and the cause of significant morbidity and mortality. As a result, OR teams are required to implement tools such as checklists, timeouts, and preop labeling – all adopted from the world of aviation.
Solutions within this category are solely focused on implementing current guidelines and improving teamwork and visibility within the operating room.
#4: Video Content Management
Conventional companies within this category have developed platforms that capture and store procedure data, empowering more surgeons to review and comment on one another’s performances. Essentially these platforms are replacing mountains of thumb drives, the modern version of a cloud-based library. But these platforms provide limited value to OR teams without unbiased, objective data analysis and integration of patient outcomes.
Finding a new way to solve surgical variability
Now we still ask ourselves, what can be done to improve surgical quality of care and efficiency on a wider scale? How can we change the sad reality of “where you live determines if you live”? How can we continuously improve surgical performance in rural hospitals and top-tier medical centers? How can we tackle surgical variability and democratize access to the best care?
Surgical variability alone is a complex challenge with many influencing factors. But those factors essentially boil down to one problem: A lack of meaningful data that allows surgeons to link specific aspects of their performance to patient outcomes.
Here’s where Theator and Surgical Intelligence come into play
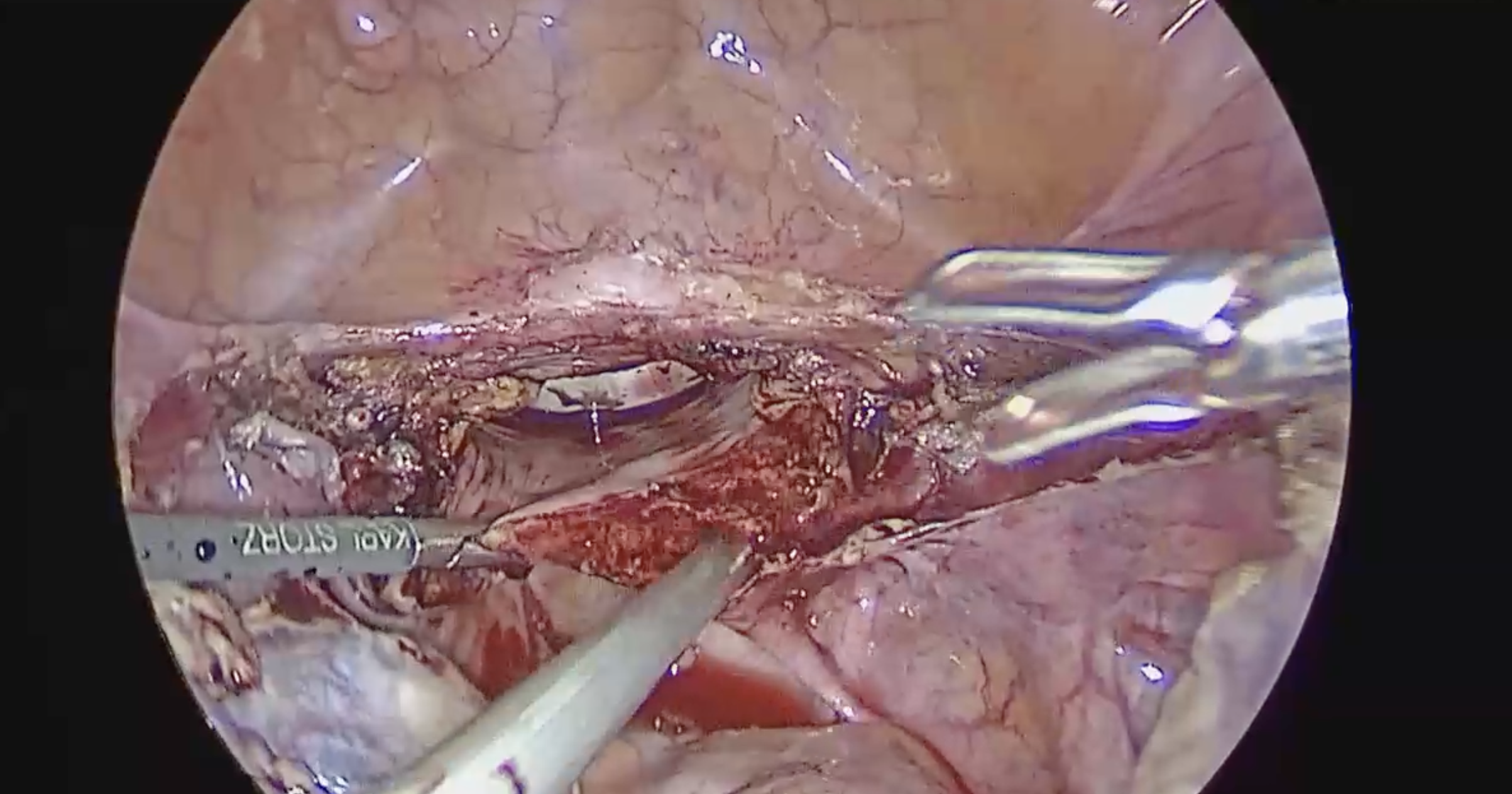
Surgical Intelligence is a new field focused on data-driven insights that improve surgical outcomes. Connecting intraoperative performance with clinical outcomes on a large scale can unearth surgical best practices. Once surgical best practices are obtained and verified, they can be disseminated and implemented worldwide.
By improving decision-making, all healthcare stakeholders understand what leads to better clinical and financial outcomes and have actionable pathways to achieving them.
At Theator, we have created the Surgical Intelligence platform.
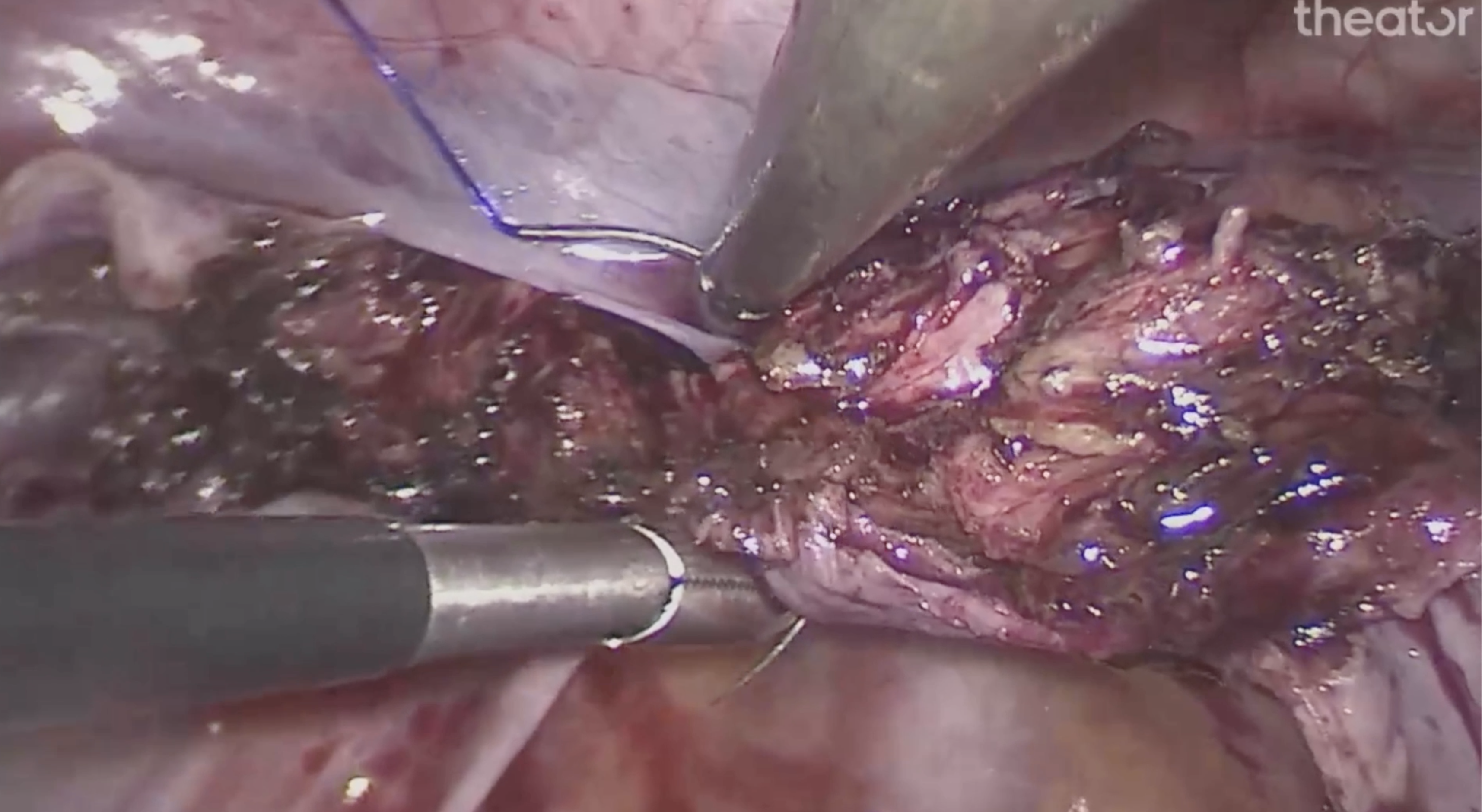
The outstanding platform captures surgical video, annotates the procedure, and analyzes it, all in real time. We’ve partnered with leading medical institutions and professional societies and continue expanding rapidly. Theator has been consistently recognized as a leader in this space, winning awards such as CBInsights top 100 AI companies and Fast Company’s top 10 most innovative companies in data science.
The part of this journey we are most proud of is hearing the positive feedback we receive from our users. Many have told us they couldn’t imagine their surgical practice without surgical intelligence. Others have improved the surgical quality in their department, positively affecting the treatment patients receive.
This is the Surgical Intelligence revolution. It’s the ideal application of “AI in Surgery” — one with immediate, practical value that empowers and supports surgeons. It’s the key to finally eliminating variability and disparities in surgical care. And, most exciting of all, it’s happening right now.