What Surgeons and Administrators Need to Know About Recording Surgical Data
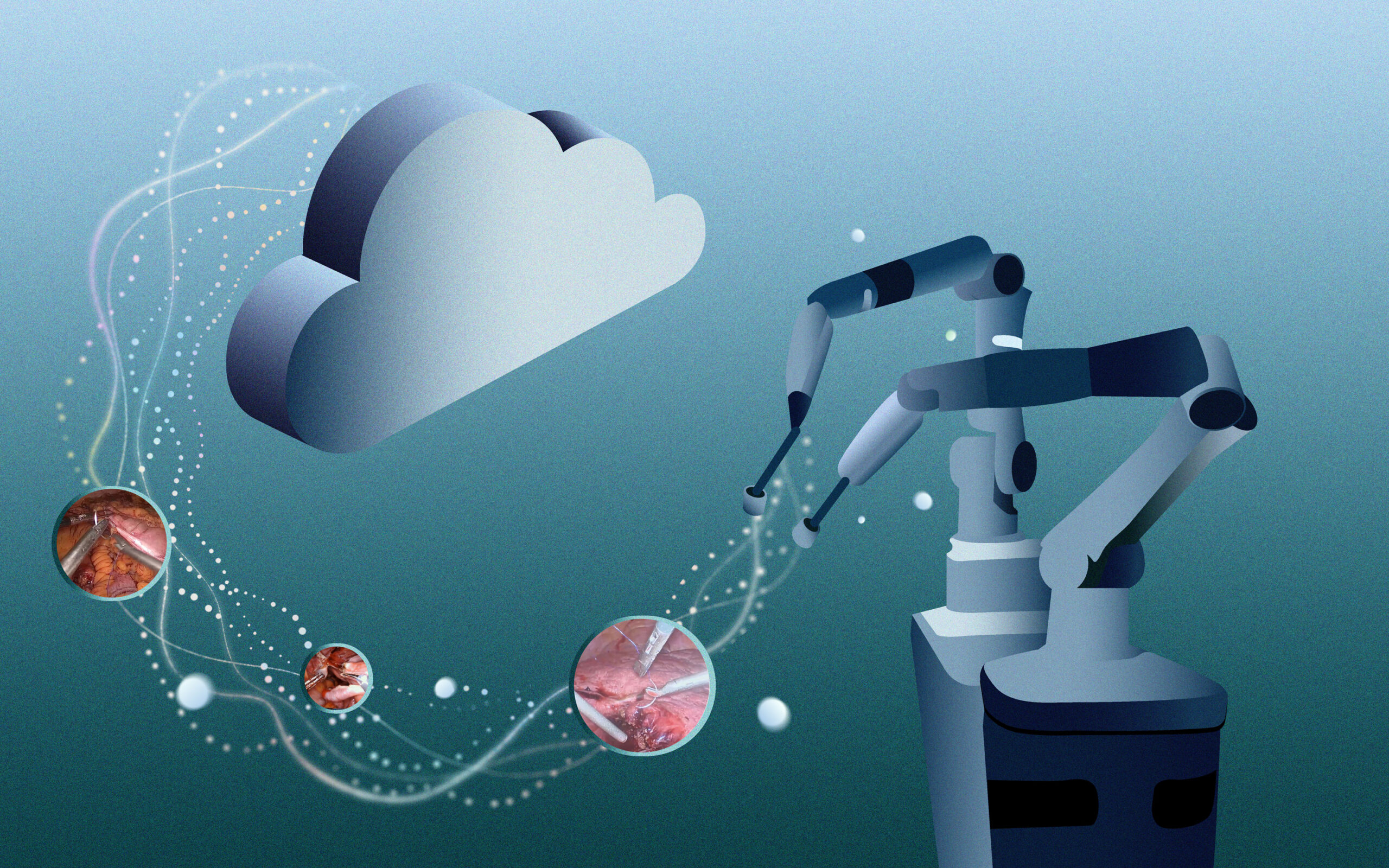
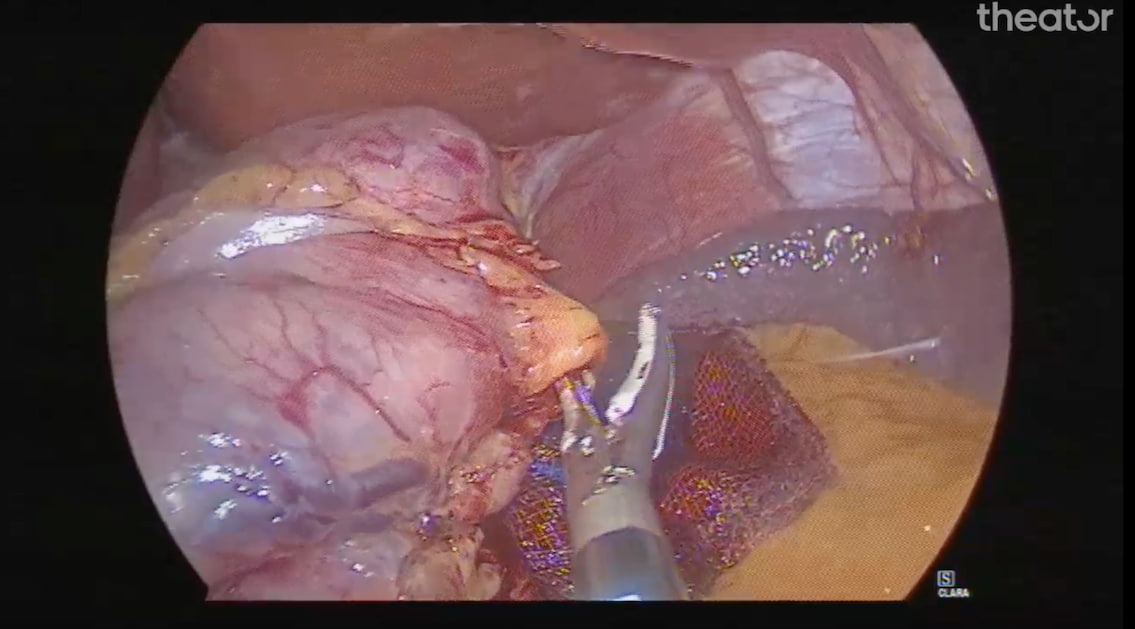
Recording intraoperative video is not a new concept, especially for those who perform laparoscopic or robotic procedures. However, as the practice of surgery continues to evolve by incorporating advanced technologies, such as AI, into everyday care, the role of intraoperative video recording will need to shift to better accommodate and advance the use of these tools.
How will this change day-to-day surgical care? What are the best ways to protect privacy and security in this new digital age of healthcare? These and other common concerns are addressed in the July 2023 recommendations published by the AI Task Force of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Read on for a breakdown of what they had to say.
Why Record (More) Intraoperative Video?
The idea of recording extensive data to improve safety originated in the aviation industry. Following highly publicized plane crashes in the 1970s, recording in-flight data became standard procedure and the systems that were put in place to address identified issues resulted in the industry achieving a near-perfect safety record.
Applying the same practices to surgical video offers the opportunity to improve patient outcomes and reduce complications in a similar manner. Importantly, recording intraoperative video is an easy process since ORs are already equipped with the necessary tools—meaning little to no valuable OR time is required to implement collection. Furthermore, currently available AI technologies are already adept at analyzing recorded video to identify surgical steps and variations, which means there is no need for surgeons to spend additional time manually reviewing recordings.
Surgical Data: Who, What, When, Where, and Why
Before implementing large-scale surgical video recording, it’s important to understand the many aspects of using and managing this data that will come into play for an organization. The SAGES AI Task Force breaks these down as follows:
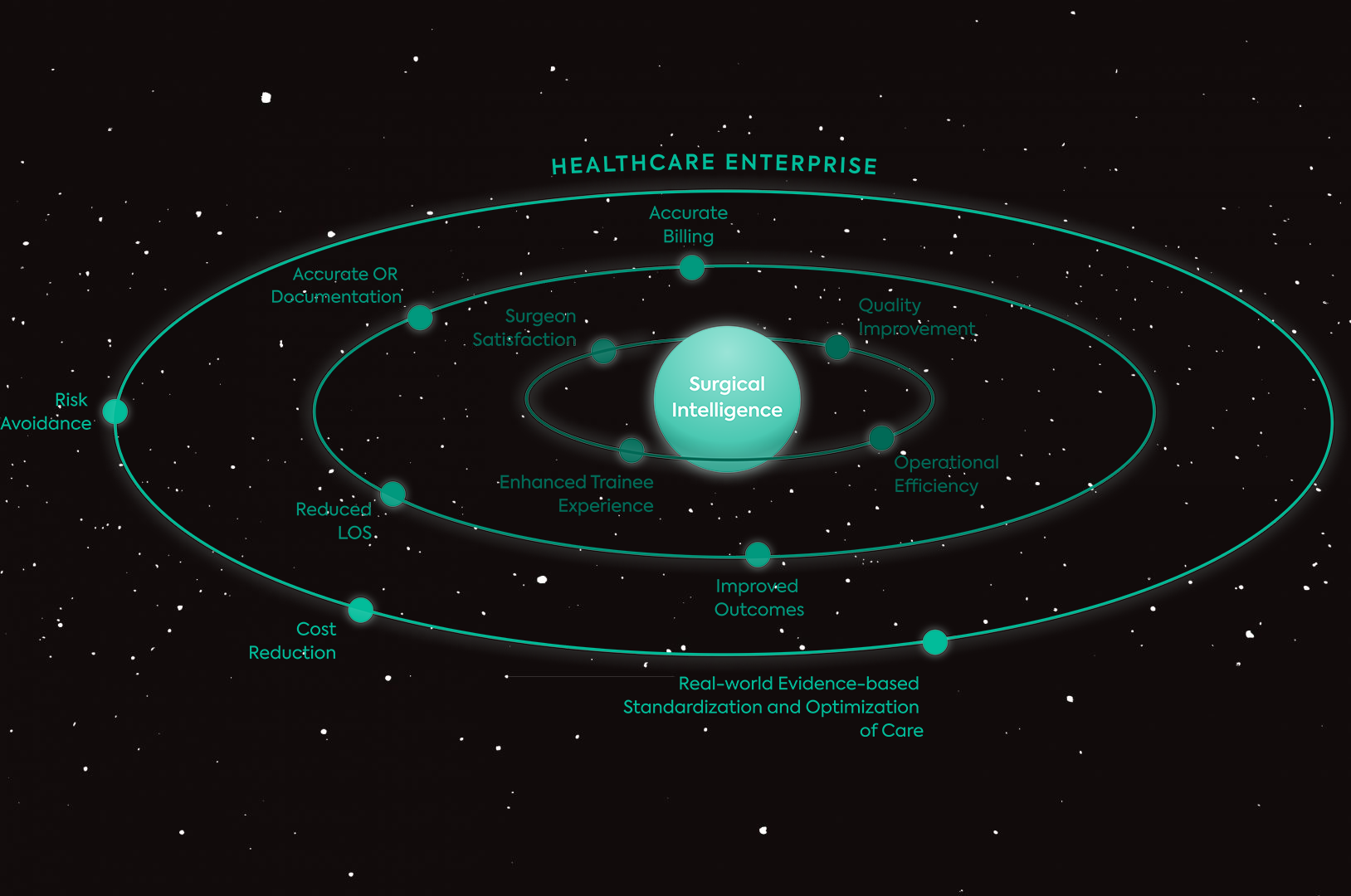
- Data Use: This refers to the need to address all stakeholders in the use of recorded data, from surgeons to patients to administrators and beyond. What does each group need from the recorded data?
- Data Structure: How will data be captured, stored, and formatted? This affects how accessible it is to stakeholders.
- Data Exploration: Once data has been collected, it’s essential to define how it will be used for research purposes to improve care and promote innovation.
- Data Governance: The ethical and legal aspects of data collection reflected in policies and procedures are key to protecting privacy and ensuring fair and just practices.
As departments, hospitals, and healthcare systems enhance their intraoperative recording capabilities and practices, all of these overlapping concepts should be proactively addressed to optimize outcomes and prevent unintended consequences.
Data Use: Who Needs the Data and Which Cases Should Be Recorded?
In terms of what and when to record, 58% of task force members felt that surgeries should always or almost always be recorded. Of note, the group pointed out the specific need to record less frequent or more complicated procedures to maximize representation of rare events for educational and quality purposes. If storage capability is a barrier to recording all surgical video, working with a technology program that offers unlimited storage can eliminate the need to pick and choose which procedures to record and simplify the process using automatic recording of all procedures.
Healthcare providers and patients were identified as the two most important stakeholders requiring access to recorded surgical data, and research, educational, and clinical use cases were all noted to be highly valuable roles of recorded data. Legal experts should be included in conversations and policy development regarding data use to ensure HIPAA compliance and address concerns related to discoverability of recorded data in medicolegal cases. In addition, attention to blurring out-of-body video segments can help to mitigate privacy concerns.
Data Structure: What Data Sources Are Most Valuable and How Should Data Be Stored?
In terms of which type of video to record, the task force felt that endoscopic data is a key addition to intraabdominal video to facilitate best practices. While using multiple sources to record intraoperative data increases the volume of available data, it also increases the need for data storage, so these two priorities should be carefully balanced. When planning an institutional approach to video recording, selection of technology that integrates with existing hardware can offer a logistically easier solution than starting from scratch with new equipment.
Quality and storage are main pillars of data structure that will require careful planning by organizations embarking on increasing their surgical data recording practices. Standardization is a vital element of this process to optimize accessibility and usability. In addition, video quality should be balanced with the intended data use, since higher quality data requires more storage. Choosing an unlimited storage platform can allow for consistent recording of high-quality data without the need to worry about running out of storage space.
Data Exploration: Addressing Bias and Furthering Research
It is well-documented that the healthcare system is fraught with bias, and it’s important that recorded surgical data not further contribute to this issue. To mitigate this, the task force suggests collecting additional data such as patient demographics and surgical team information to provide context to recorded data. Because recorded data are used to train AI algorithms, reducing bias in recorded data can ultimately reduce bias in these algorithms.
Planning for surgical data collection and storage should not only consider the current uses for this data, but also the potential future uses for safety and quality improvement, research, and outcomes analysis. This approach can inform forward-thinking practices for data management.
Data Governance: The Laws and Ethics of Data Collection and Storage
Transparency is key to the development of data governance policies that align with the principles of medical ethics. Patients should be informed about the use of video recording and have the opportunity to consent or decline the use of intraoperative recording.
Related to this, access to recorded surgical data should be managed in a way that protects patient privacy and limits its use to predetermined use cases. Involvement of ethics boards and institutional review boards is encouraged to facilitate best practices in this area.
Institute Policies Today to Be Prepared Tomorrow
The use of advanced technologies, such as AI tools, in the OR is on track to quickly become the standard of surgical care. The first step in implementing such technologies and their advantages is the collection of recorded intraoperative data. Luckily, ORs are already equipped with the tools to do this, so getting started is easy. However, the storage of large volumes of data, identification of its intended use, and privacy and security compliance are critical areas of consideration that should be planned for—purposefully and strategically that include all stakeholders—before embarking on large-scale data collection.