From Innovation To Impact
![]() Jordan
on
September 27, 2024
Jordan
on
September 27, 2024
Why value must lead in healthcare
In today’s world, innovations in the healthcare space need to show value immediately. Gone are the days when health systems were willing to adopt new technology that promises value. Rightfully so, health systems today require examples of both short-term and long-term value before adopting a new technology.
Surgical Intelligence in Action
Advanced technology like artificial intelligence (AI) is not new in the surgical field. Surgical intelligence, however, is still in its infancy, and there are multiple schools of thought on what applications and data sources should be leveraged to provide the most value. But, one thing is consistent, examples of how value has been demonstrated is necessary.
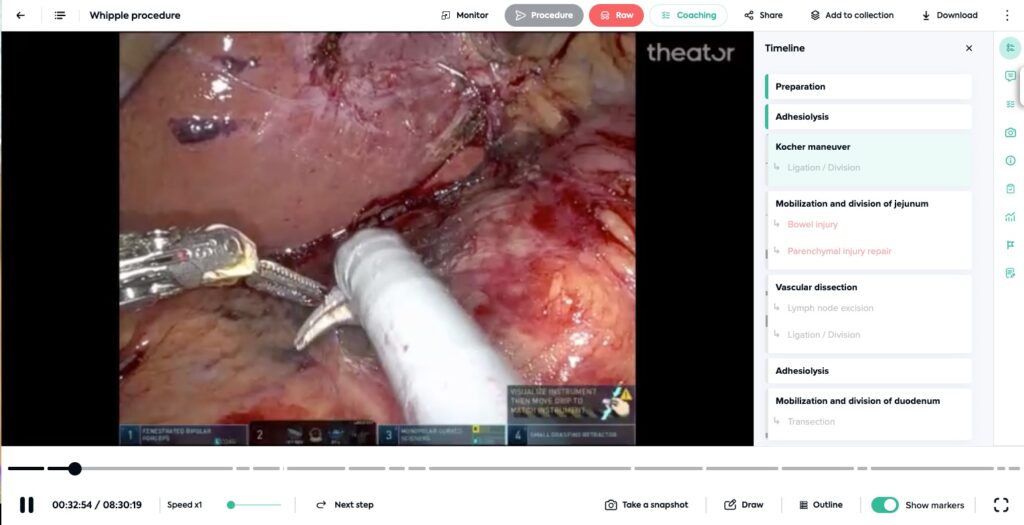
Let’s start with just the surgical video alone. Capturing, structuring, and analyzing surgical video unlocks unique insights that set the foundation for larger-scale, comprehensive impact. Leveraging Theator, our partners have improved surgical quality, reduced operating time, and accelerated training. Let’s dive into each one of these.
Example 1: improving the quality of patient care
We have seen a variety of approaches in surgical-intelligence-driven quality improvement, some proactive, and some reactive. A common place for our partners to start is to surface where low adoption to surgical practices that increase the quality of a procedure exist and create a proactive quality initiative to drive an increase in department-wide adoption. Time and time again, we see significant adoption increase over the course of a few short months.
Example 2: reducing operative time
Operative time can be analyzed in a few ways – total procedure duration, per-step duration, and also idle time (both in-body and out-of-body). All of these time elements are important to driving consistent and predictable OR scheduling, and, managing OR costs as every minute counts. Structuring and analyzing this data has shown our partners where and why significant idle time is contributing to increased operative time, where outliers exist to drive standardization and more.
Example 3: accelerate education for trainees
Have you ever asked a surgical trainee what resource they use to prep for a surgical procedure? The answer is probably not their medical school textbooks. Rather, the answer is likely YouTube. We know video is a valuable learning tool. Now, with surgical intelligence, trainers can specify which videos to review, provide constructive feedback on specific parts of the video in which a trainee operated, and collaborate in so many more ways.
These examples are just the beginning of surgical intelligence. To read even more, download this booklet to read through some of our favorite examples of how our partners are demonstrating value every day with surgical intelligence.