Surgical Spotlight: Robotic vs. Laparoscopic Hysterectomy
![]() Theator
on
July 16, 2024
Theator
on
July 16, 2024
Robotic vs. Laparoscopic Hysterectomy
Gynecologists were among the second specialty of surgeons to widely adopt a robotic-assisted approach. One of the first robotic-assisted hysterectomies was performed by Dr. Advincula in 2001. Fast forward to 2020, and robotic adoption for hysterectomies has jumped to 30% for benign cases and 65% for oncologic diseases.
So, is laparoscopic “better” than robotic? Or vice-versa? Or, does it depend on the type of case?
We aren’t here to answer that. But, in reviewing 1,795 cases, we did spot a few differences, empowering hospitals and surgeons with real-world data to inform their own, data-driven decisions. Download the report here.
Variability in procedure time
Overall, robotic hysterectomies take 39% longer than laparoscopic cases. In particular, one step accounts for the majority of that increased time adding a median of 18min to cases.
Variability in Surgical Practice to Enhance Quality (SPEQ)
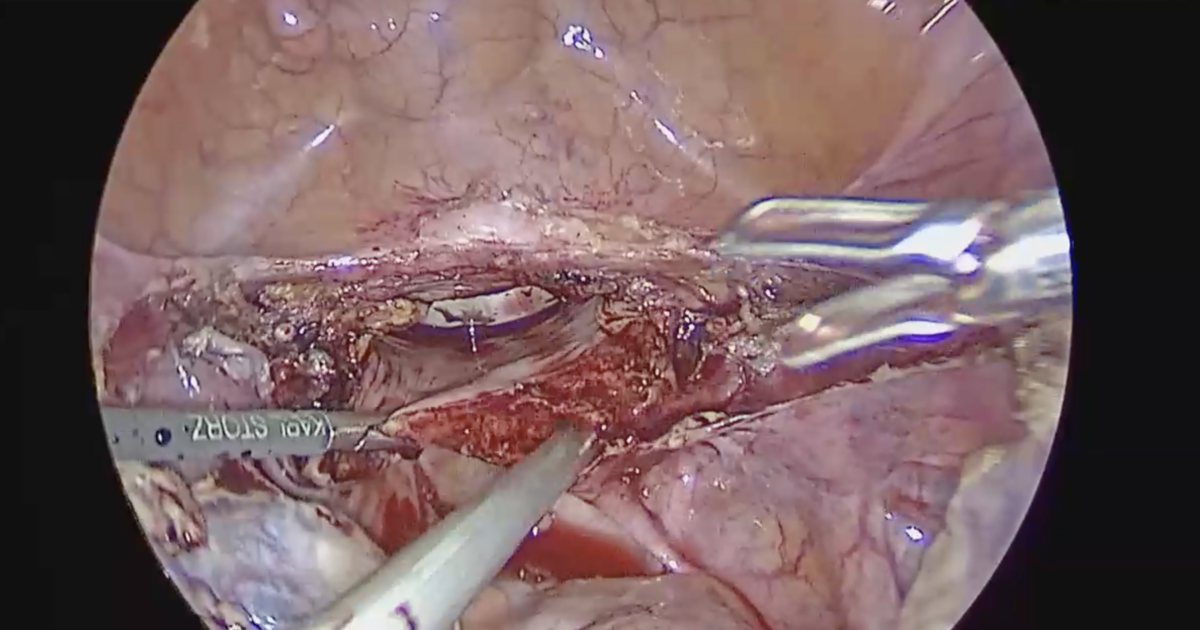
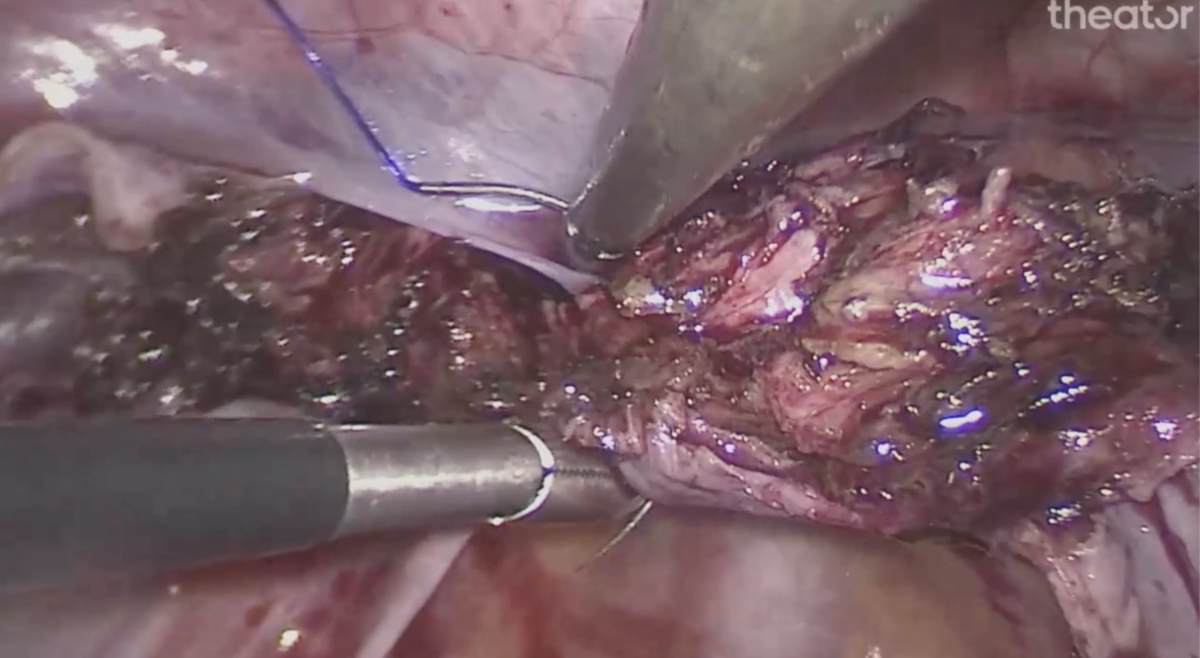
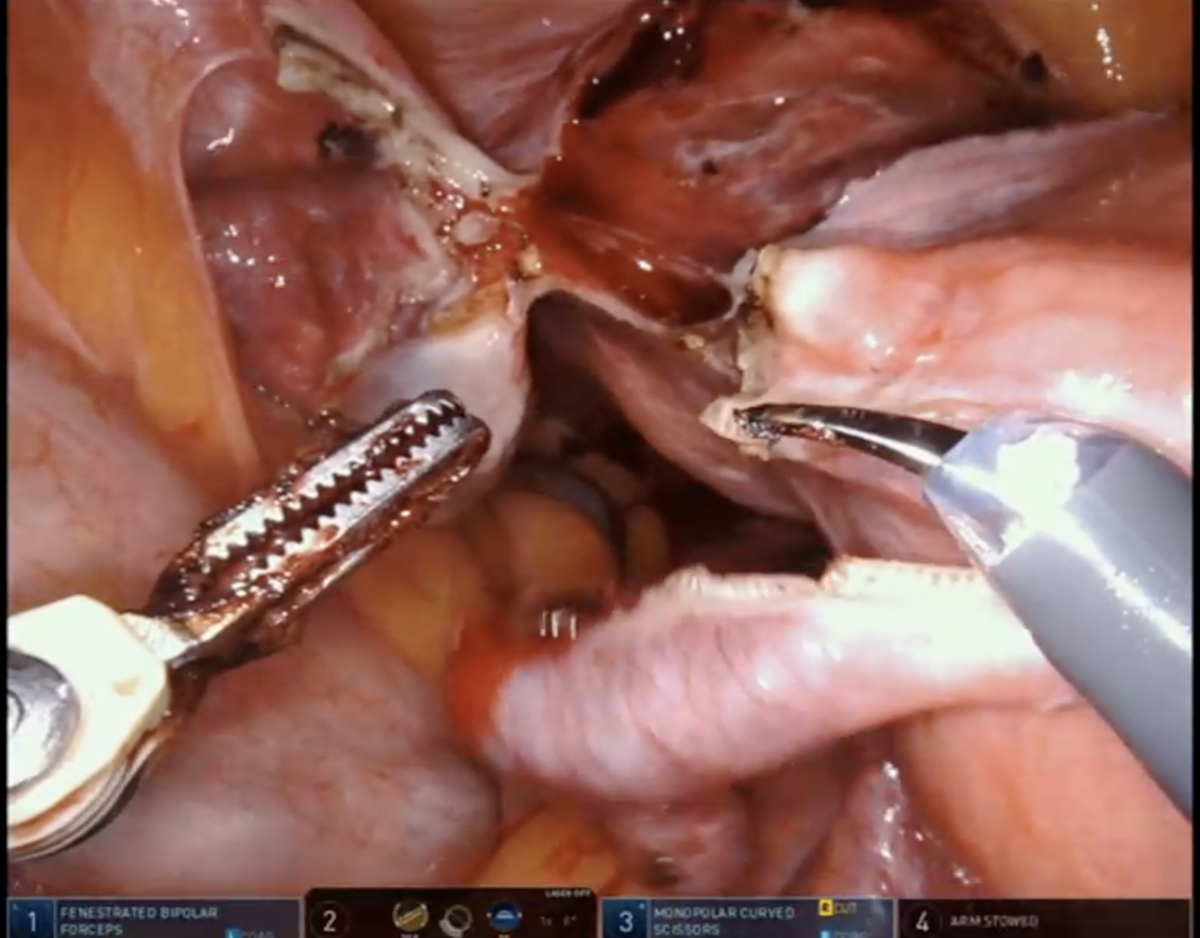
Identification of critical anatomic landmarks is an essential step in preventing surgical complications associated with laparoscopic hysterectomy. For example, one SPEQ – identification of the bilateral ureters – can prevent injury to these structures. And, interestingly, view of ureter was achieved significantly more frequently.
Despite an overall increase in achievement of view of ureter in robotic cases, that wasn’t necessarily true in all of the health systems included in this analysis.
Check out the full report to see variability across and within health systems.