Surgical Spotlight: Robotic vs. Laparoscopic Sleeve Gastrectomy
![]() Theator
on
July 23, 2024
Theator
on
July 23, 2024
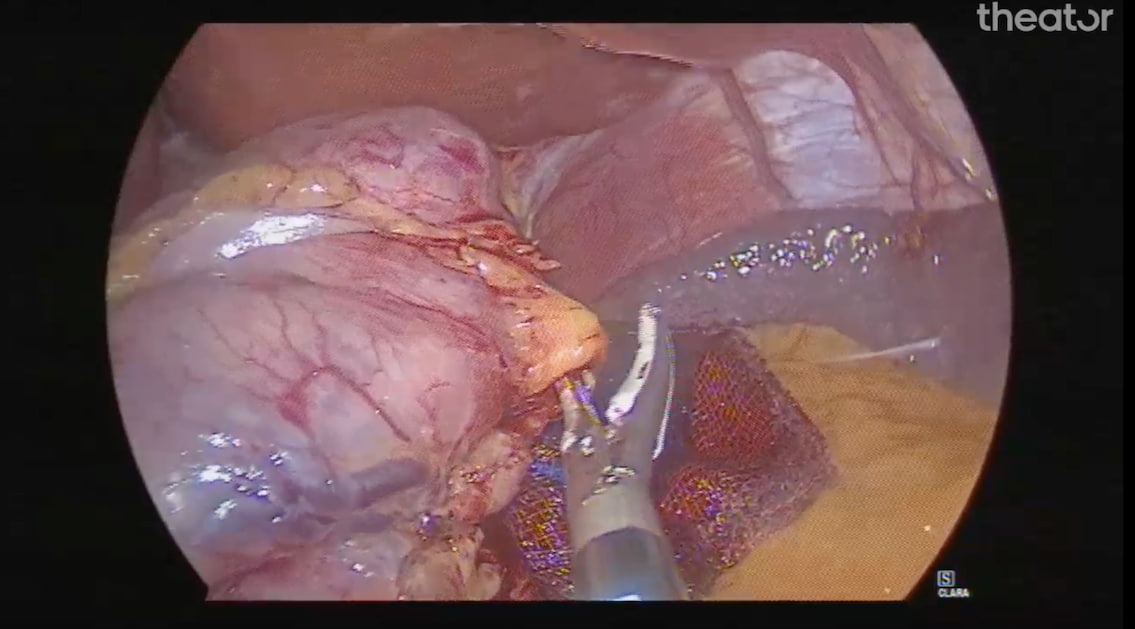
Robotic vs. Laparoscopic Sleeve Gastrectomy
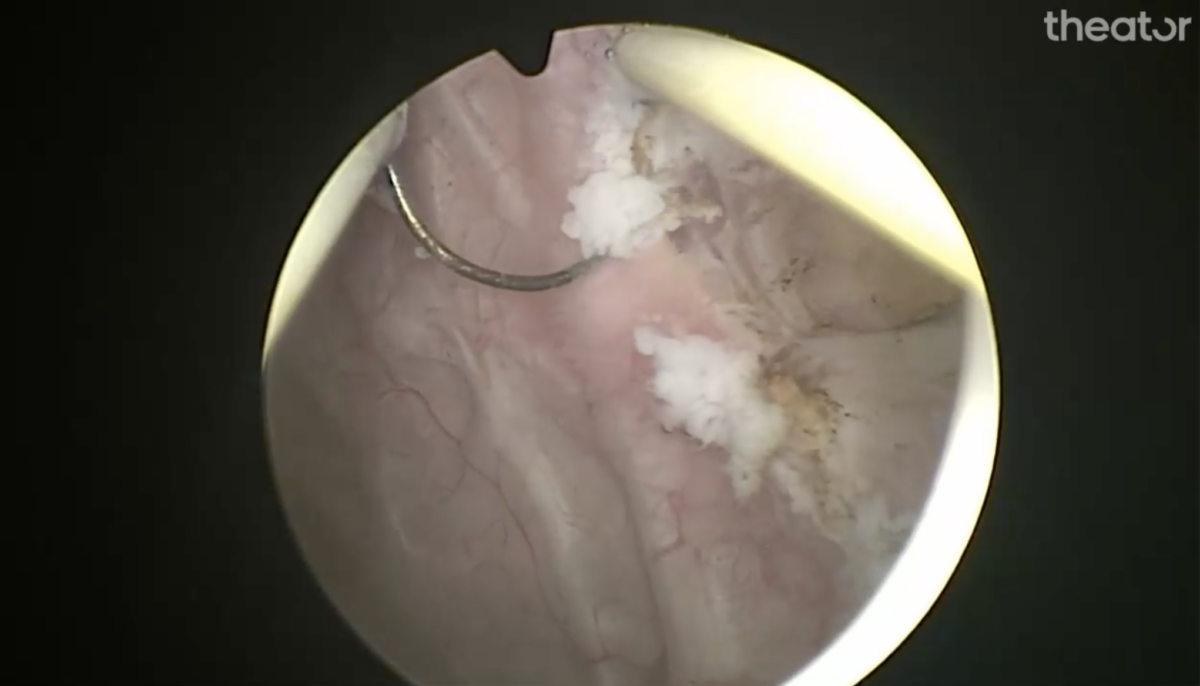
Sleeve gastrectomy, also known as gastric sleeve surgery, is a frequently performed weight loss surgery that removes 80% of the stomach, leaving a much smaller organ that holds less food and liquid. A further advantage of this procedure is that the portion of the stomach that produces a hunger-inducing hormone is removed, leading to a decreased appetite and improved metabolism.
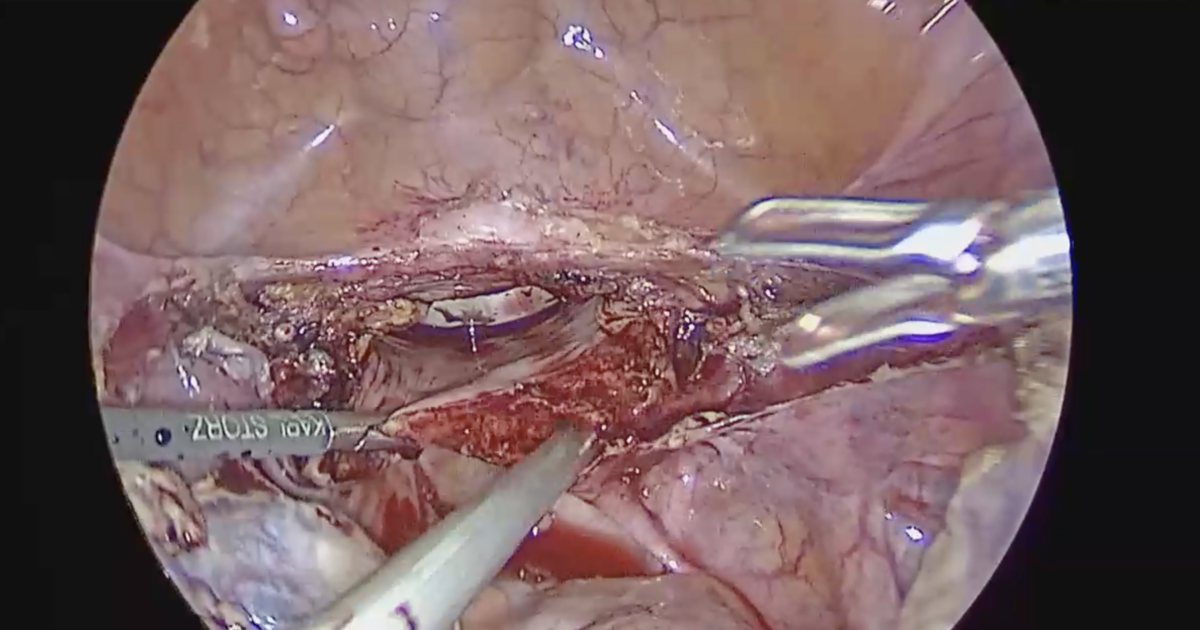
While this procedure was traditionally performed laparoscopically, in recent years more surgeons are performing robotic-assisted sleeve gastrectomies.
What’s the difference between laparoscopic and robotic-assisted sleeve gastrectomies? We’re glad you asked. In general, the main benefits of robotic-assisted surgery include a clearer view for surgeons, high accuracy of movement, and reduced trauma, meaning less tissue damage, bleeding, and pain.
Does this mean that robotic-assisted sleeve gastrectomy is the better choice? Not necessarily. Read on to find out what we learned from analyzing 505 surgical videos across a health system.
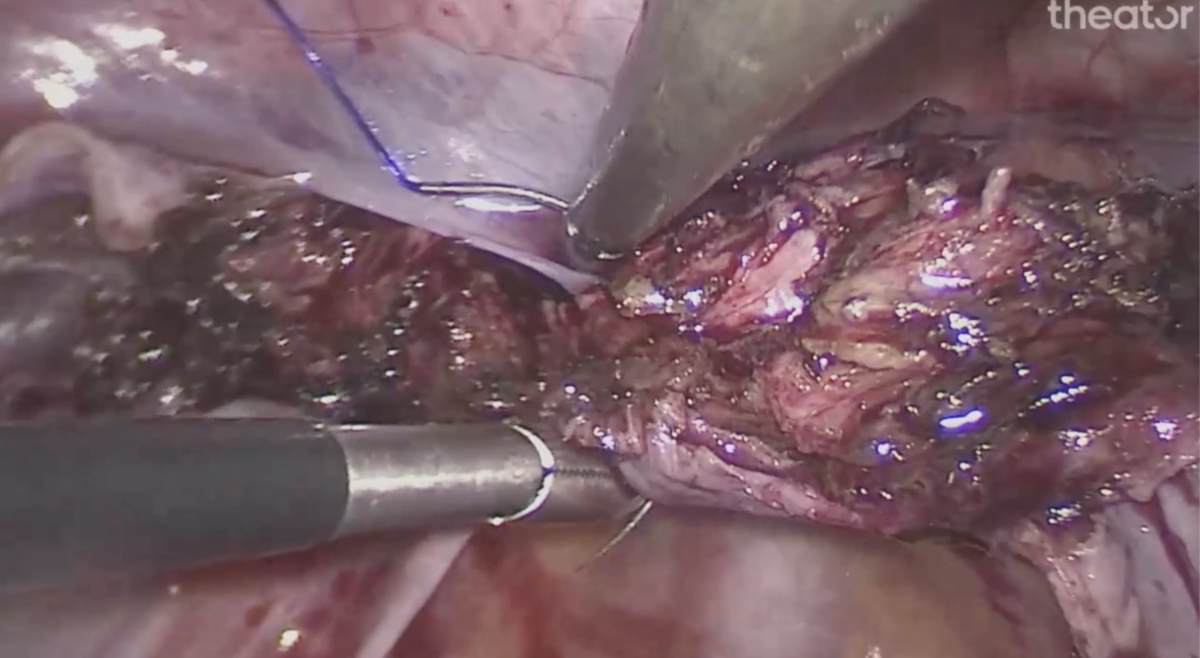
Longer Operative Times
While many aspects of surgical care affect patient outcomes, longer operative times have been associated with increased chances of complications. In the case of sleeve gastrectomy, you likely won’t be surprised to learn which approach is associated with longer operative times (*cough* robotic *cough*). But it may surprise you which procedure step is the biggest contributor to that increase in median operative time.
Download our Spotlight report to learn more.
This is just one of many data points that Theator’s Surgical Intelligence Platform automatically recognizes, analyzes, and delivers back to to health systems in digestible formats so hospital administrators and surgeons can take a data-driven approach to improving the quality of surgical care.
Curious to know more about the differences in operative time between the two approaches? We have the answer. Download the full report here.