Surgical Spotlight: Right Hemicolectomy
![]() Theator
on
May 22, 2024
Theator
on
May 22, 2024
One colorectal procedure, and the postoperative complications that can happen
Right hemicolectomy is a common colorectal surgical procedure to treat both benign and malignant conditions, including inflammatory bowel disease, colon cancer, and diverticulitis. While surgery is often a necessary step in a patient’s treatment plan, these cases don’t always go as planned.
What do we know about postoperative complications with right hemicolectomy? We know they can occur shortly after surgery or later in the postoperative course. We also know that early complications include:
- Anastomotic leaks
- Infections
- Bowel obstruction
- Bleeding
- Cardiopulmonary complications
Many factors can impact whether or not a patient experiences a complication. When looking at the right hemicolectomy surgery itself, there are 6 surgical practices Theator automatically identifies and annotates, all associated with reducing the risk of one or more postoperative complications.
Reducing anastomotic leaks in right hemicolectomies
Let’s dive into one complication, in particular. Anastomotic leaks occur in 6.4% to 8.8% of cases and can contribute to postoperative mortality and the need for revisional surgeries. Anastomotic leaks also increase healthcare costs and can lead to worse functional and oncologic outcomes for patients. Surgeons and hospital administrators want to reduce these, first and foremost to help patients.
What can surgeons do during surgery to reduce the risk of postoperative leaks?
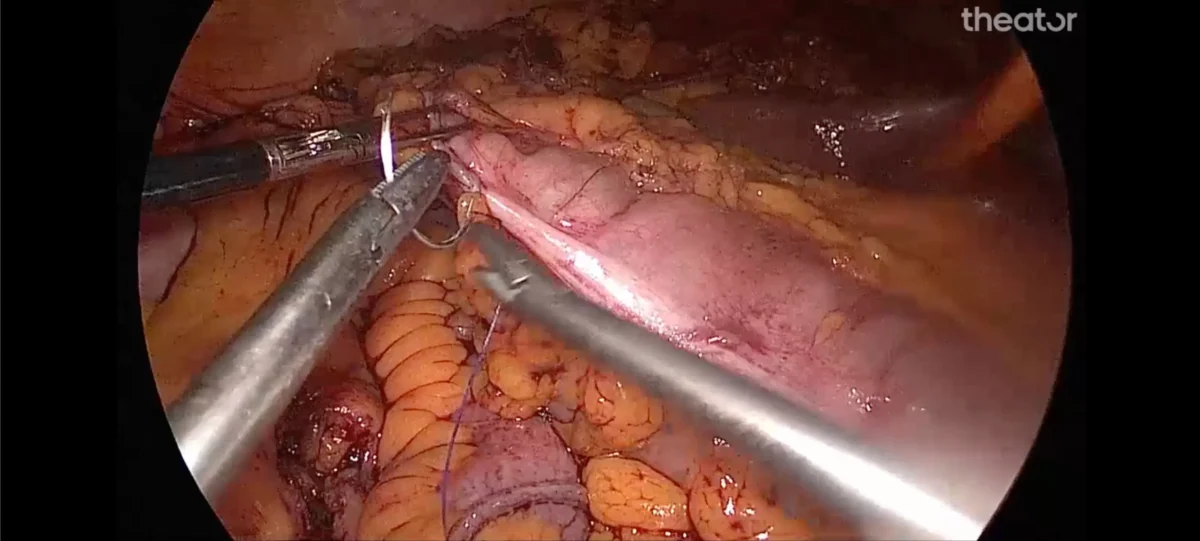
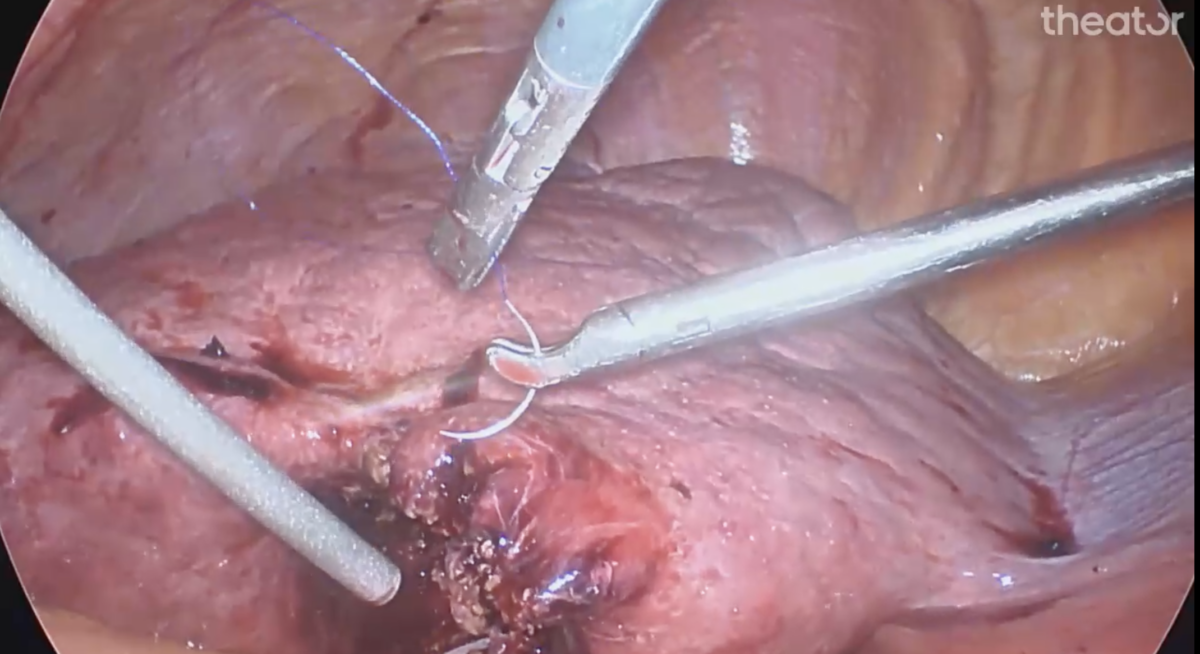
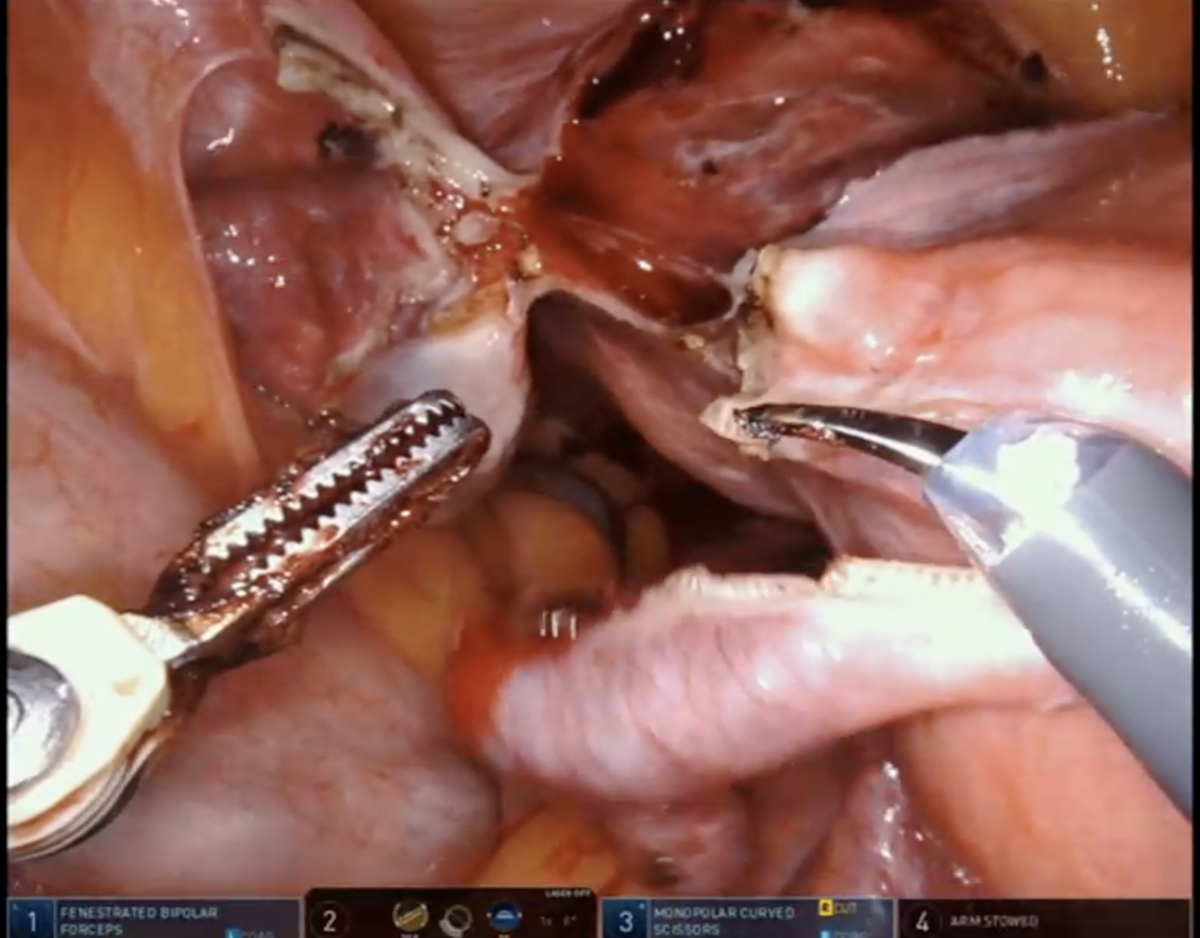
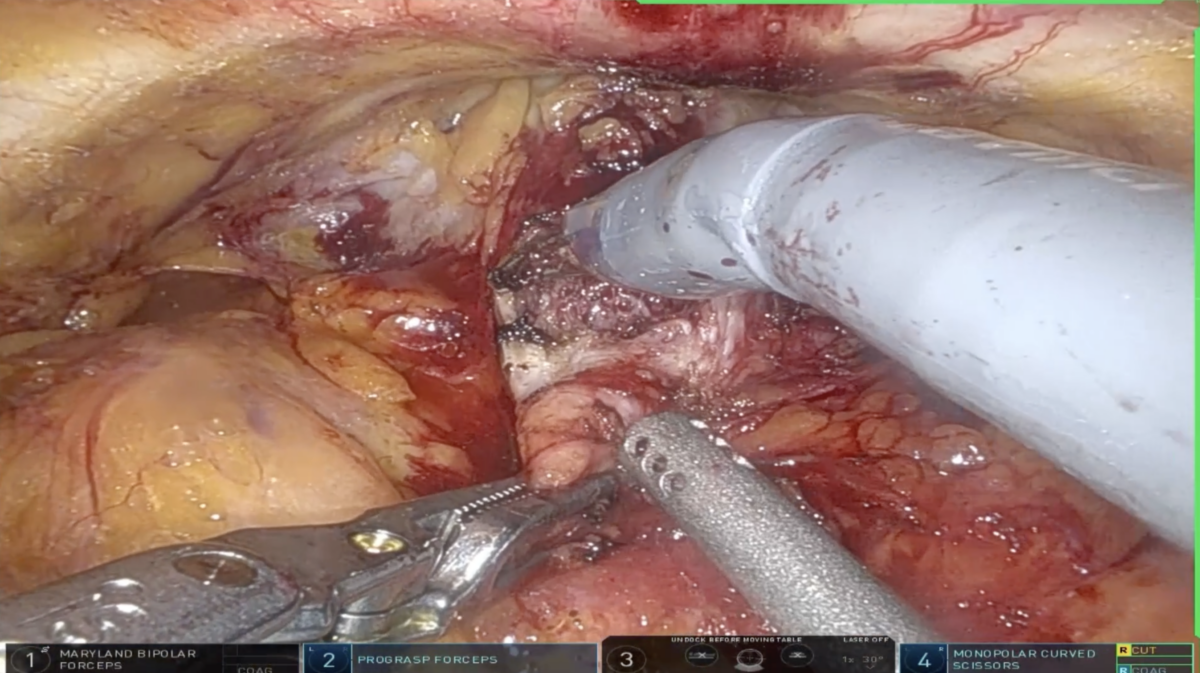
Some literature suggests that performing the anastomosis in right hemicolectomy intracorporeally instead of extracorporeally is associated with several improved outcomes. This includes potentially lower rates of anastomotic leak and reduced rates of incisional hernias, open conversion, reoperation, blood loss, and incision length.
So, we asked the question – how often is intracorporeal anastomosis performed across health systems? The answer is less than you think.
How often is intracorporeal anastomosis performed in right hemicolectomies?
Intracorporeal anastomosis was only performed in 54% of cases.
Theator’s Spotlight database has compiled nearly 400 right hemicolectomy procedures from 6 different health systems to investigate.
This is just one of many surgical practices that Theator’s Surgical Intelligence Platform recognizes, analyzes, and connects to health system outcomes so hospital administrators and surgeons can take a data-driven approach to improving the quality of surgical care.
Curious to know how the adoption of this surgical practice varied between the 6 health systems? What about between hospitals within the same health system? We have answers. Download the full report here.