Robot-Assisted Radical Prostatectomy Insights
Prostate cancer is the second most common cancer in men, with an estimated 288k new cases diagnosed in the US every year, and an estimated 34k deaths per year as a result of it.
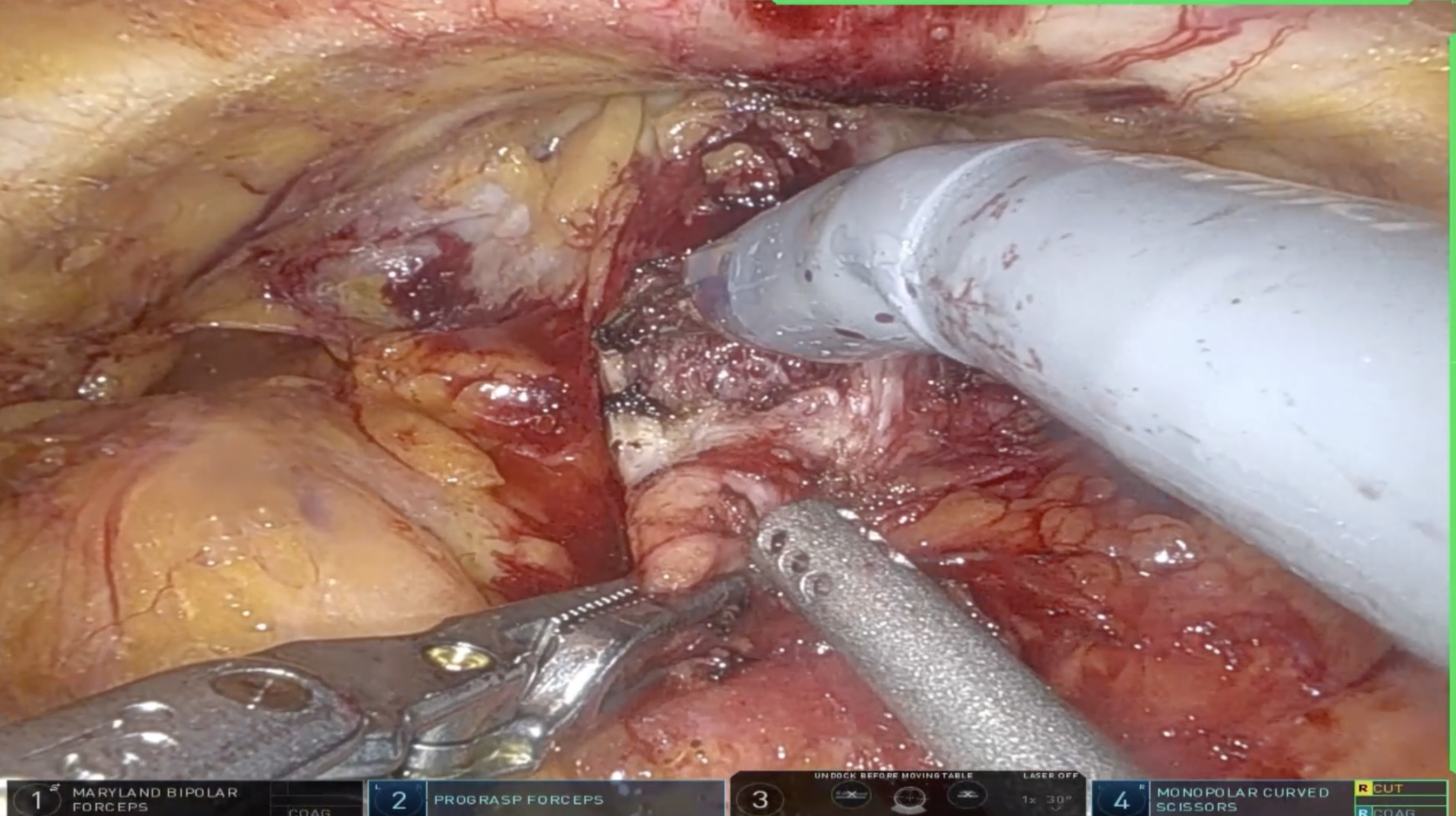
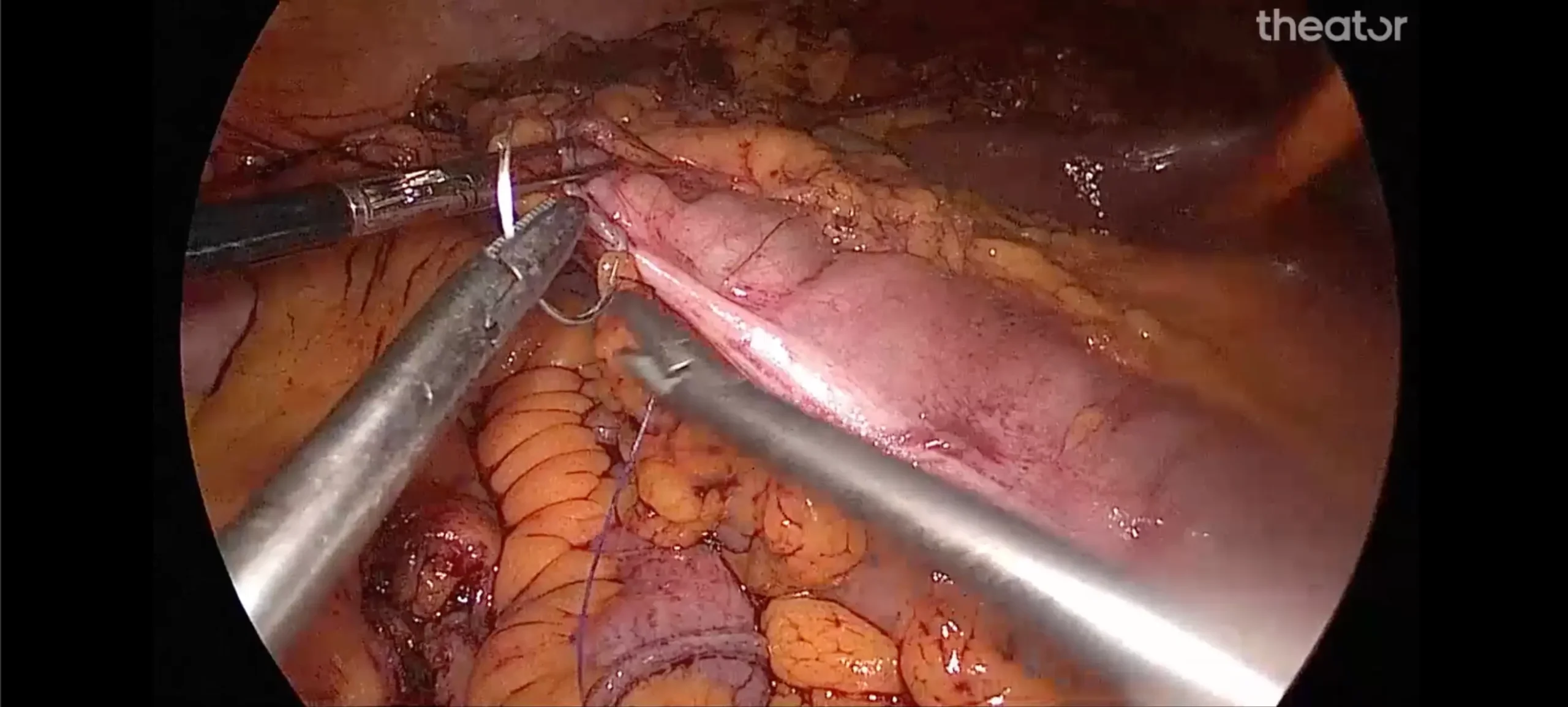
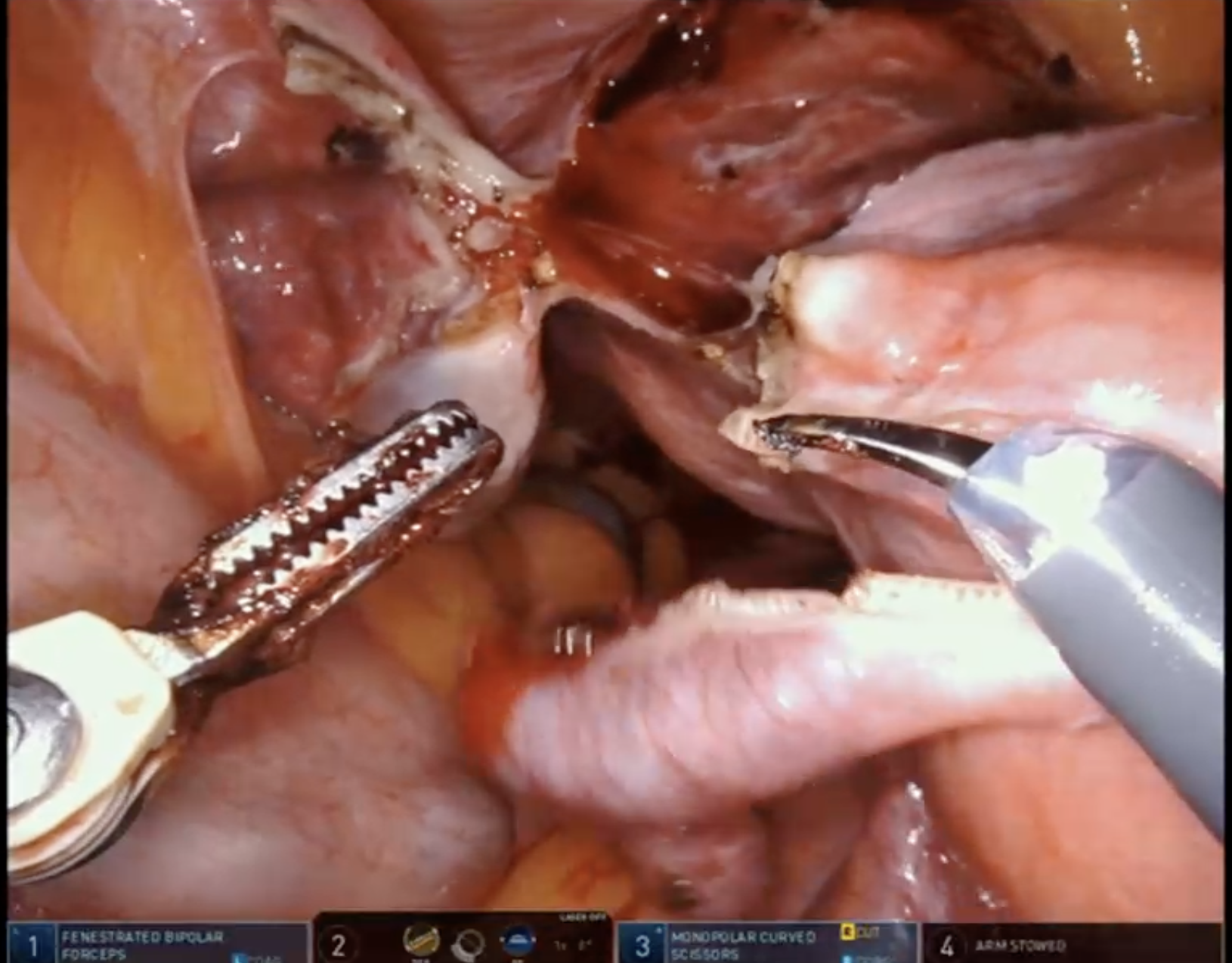
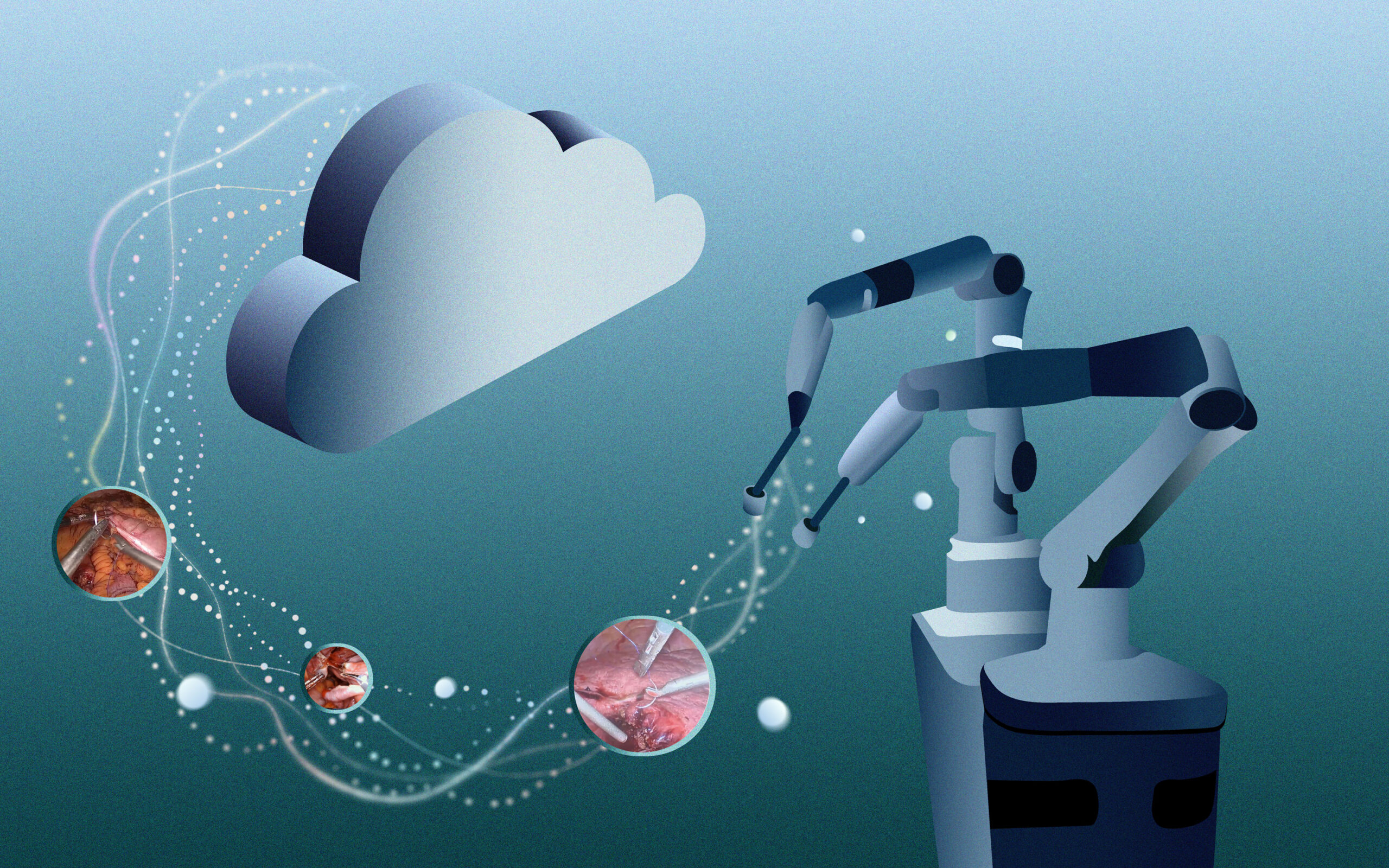
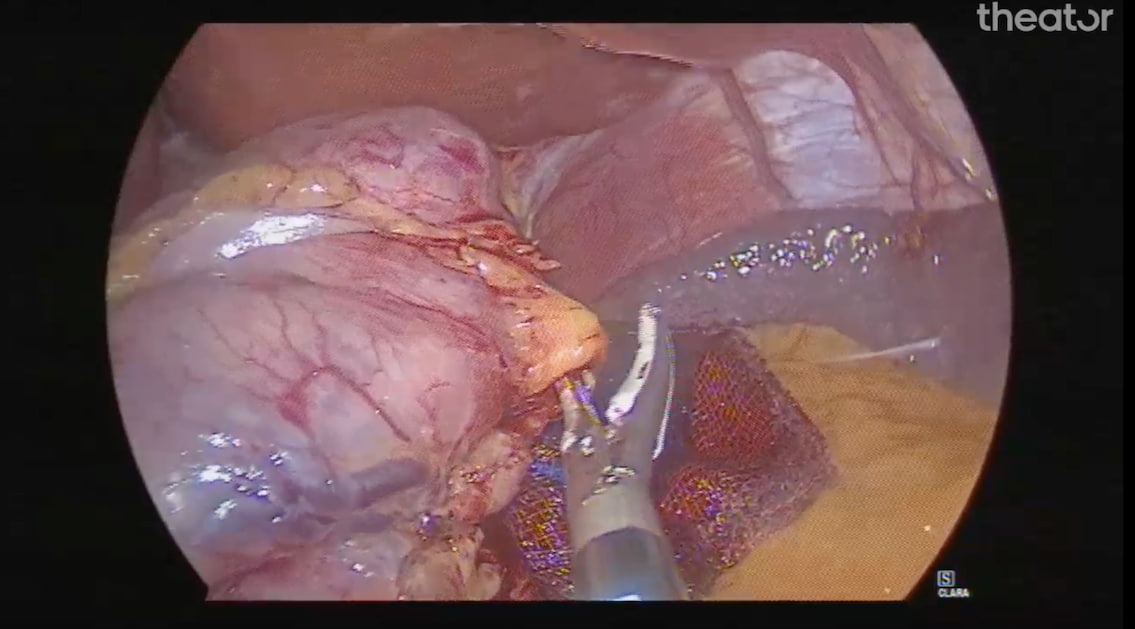
Robot-assisted radical prostatectomy (RARP) has been a treatment option for men with intermediate to high-risk prostate cancer since 2001. Theator’s Surgical Intelligence database has compiled more than 750 RARP procedures to date, from 6 different health systems.
Like any surgical procedure, RARP has potential complications, including:
- bleeding/vascular complications (1.9-6.8% of cases)
- urinary incontinence (4-31% of cases)
- erectile dysfunction (10% of cases)
In the 5 years following RARP, 17% of patients are readmitted. The most common reasons are:
- Urinary obstruction (73%)
- Urinary infection (13.5%)
- Bleeding (6%)
In addition to the physical and emotional impact on patients in these cases, hospitals incur significant costs.
For more RARP insights, download our procedure spotlight report >>
Surgical Practices in Robot-assisted Radical Prostatectomies
You might think a surgery that has been done for decades would be standardized with surgeons from all over the world performing the same steps and same surgical practices. Unfortunately, this is far from the truth.
Not only are surgical practices not agreed upon, there’s very little data to support which approach or which techniques consistently optimize outcomes.
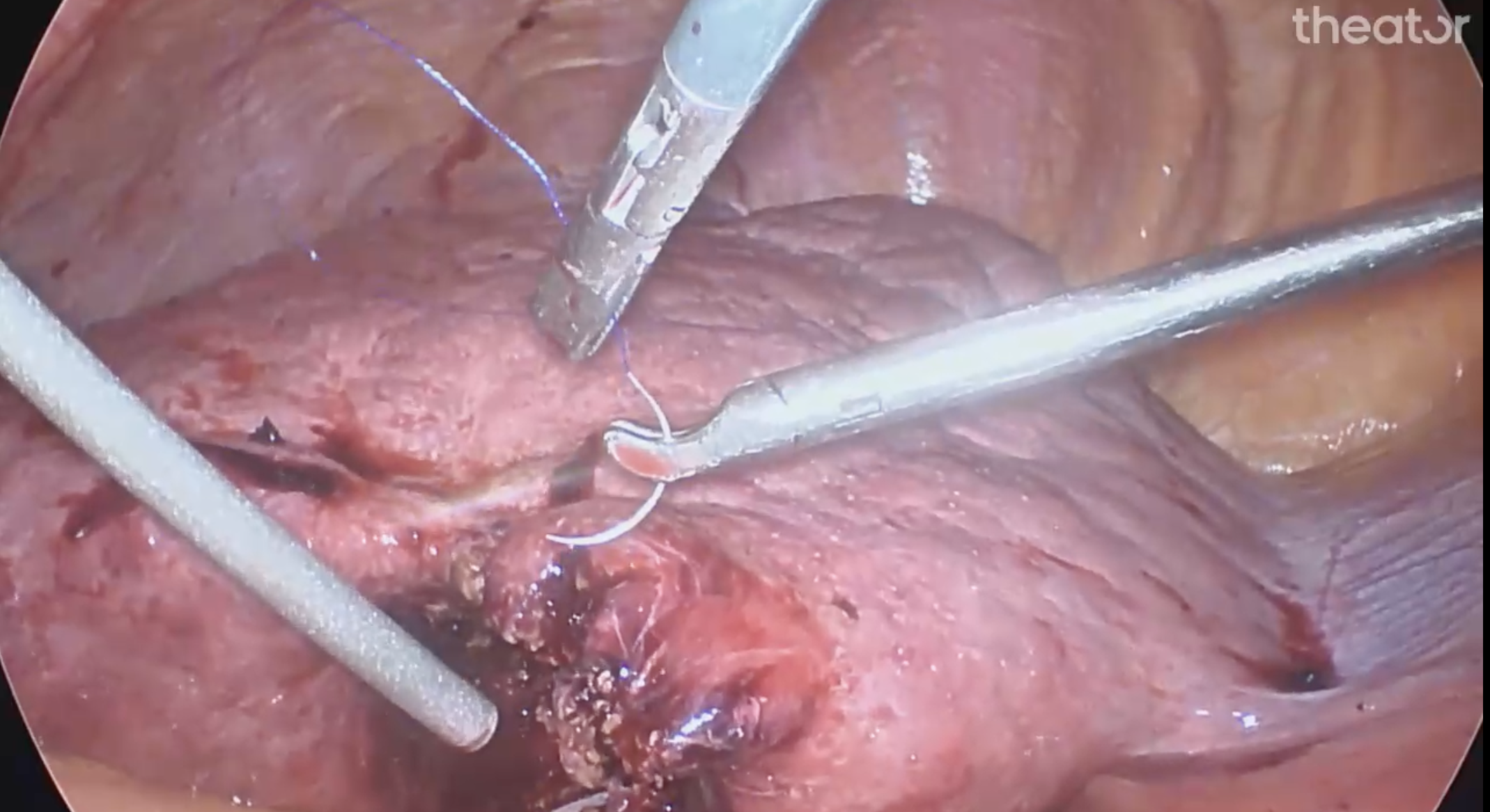
For example, one surgical practice, bladder neck suture, is performed 9% of the time at one health system, and 50% of the time at another. Which begs the question: why the variability?
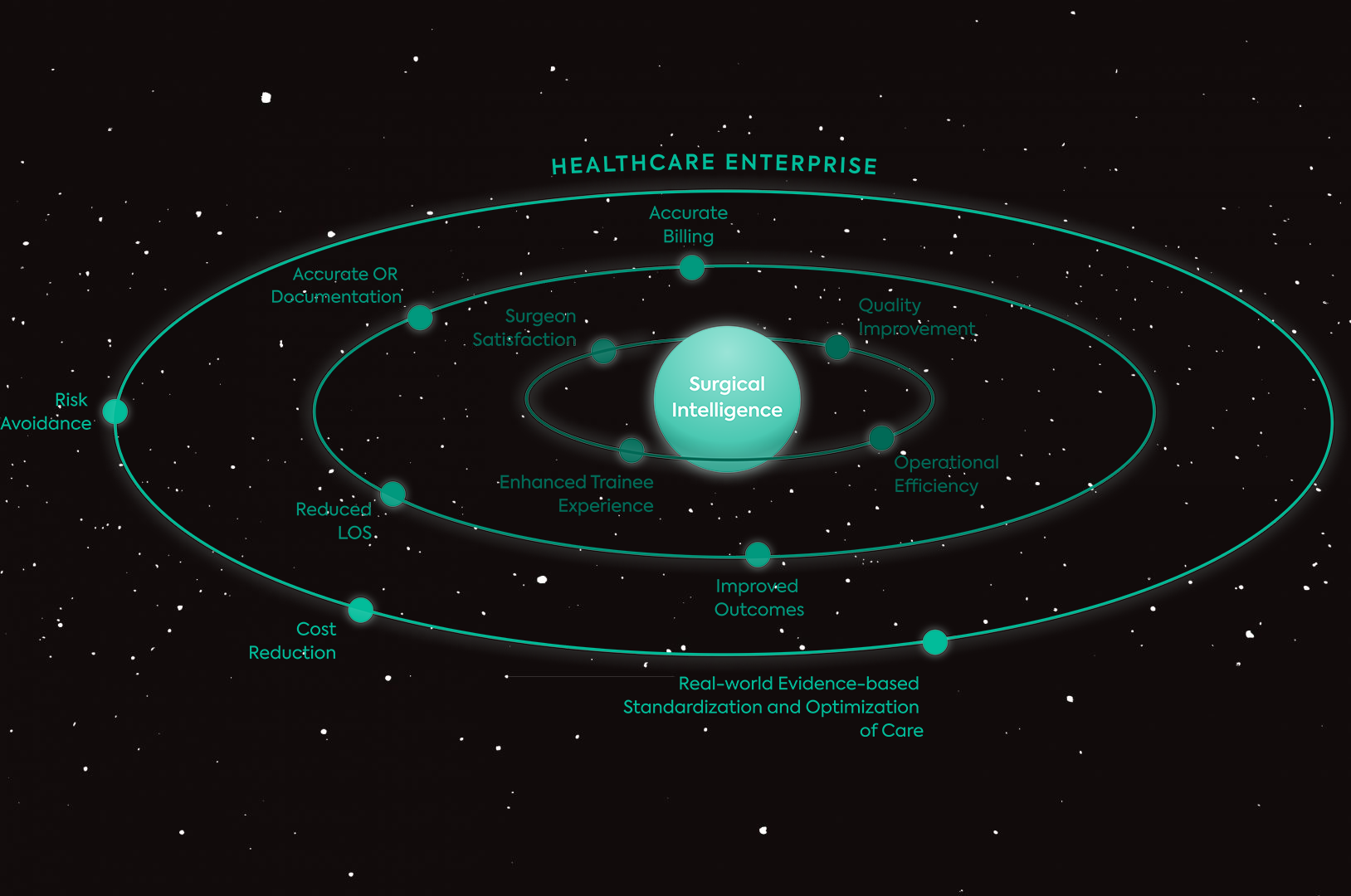
This is just one metric that Theator’s Surgical Intelligence Platform recognizes and analyzes across a health system and connects it to outcomes, so hospital administrators and surgeons alike can take a data-driven approach to improving the quality of surgery.
Curious to know what other insights we’ve seen in our database of RARP surgeries? Download the full report here