Simply capturing surgical video isn’t enough
Surgical video capture is not new. It’s been around for quite some time, and as expected, many surgical camera vendors have their own capture solutions. They have varying levels of automation and widely varying technological capabilities, but they all serve a similar purpose – to help sell more cameras. Meaning most of these solutions are not compatible with hardware other than their own This problem can be easily solved, by moving towards one vendor-agnostic software to capture all video, automatically, and with advantage technological capabilities.
Surgical videos need to be structured to make sense
Do surgeons have time to review hours of surgical video after performing hours of surgery? Of course not. But if the video is structured, surgeons can review key moments in minutes, not hours.
Do hospital administrators analyze surgeries based on written operative reports to surface trends to drive improved safety or operational efficiency? Likely so, but misalignment between written operative reports and surgical video is a widely known reality.
Leveraging the power of advanced artificial intelligence (AI) and computer vision, hundreds of procedures can be automatically structured with procedure steps, intraoperative events, surgical practices, idle time, instruments, and more. Saving surgeons time, and providing more accuracy to administrators.
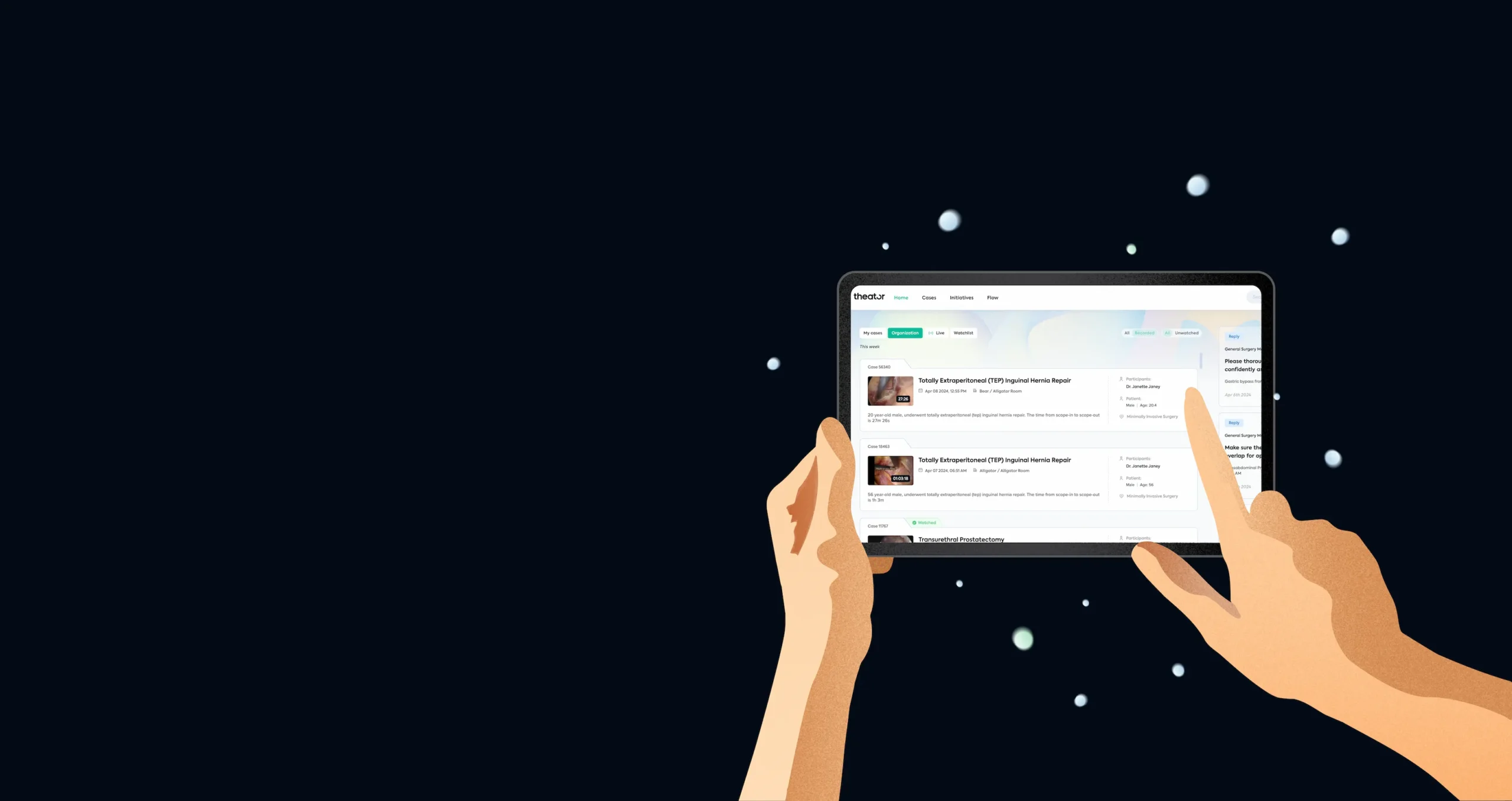
Turns out, we can learn a lot from structured video alone
Structuring and analyzing surgical video drives clinical, operational, and educational value, but surgeons and hospital administrators don’t have the time or resources to dive through tons of data. They need it to be presented to them in a digestible format. How does this actually work in the real-world?
Let’s take a look at one example for each of these value drivers:
Clinical and operational value: Safer procedures, performed more efficiently
Most procedures have surgical best practices (SBPs) and surgical practices that enhance quality (SPEQs). Adoption of SBPs and SPEQs are now being understood for the first time, thanks to automated identification with the power of AI and computer vision. Not surprisingly, adoption is lower than surgeons and hospitals expect. Several examples across multiple specialties show an increase in adoption to just one SBP or SPEQ consistently reduces operative time by 12-25%. Yes, you read that right. Higher quality procedures, performed faster. A win-win.
Specifically, in laparoscopic cholecystectomy, one hospital saw a 77% increase in SBP adoption while reducing operative time by 28%, in just 8 months. That’s just one procedure, in one specialty, in one hospital. Imagine this compounded across specialties, across hospitals all over the world. A global win-win.
Educational value: A 3x increase in surgical video feedback
A large US-based academic medical center with 1,400 beds across 18 hospitals wanted to accelerate training for their urologic surgery residents. The residents also wanted more regular and actionable feedback. With surgical videos now automatically captured and, importantly, structured (surgical steps, intraoperative events, surgical practices, and more), the department saw a 3x increase in surgical video review over the course of six months.
Next up: outcome data
With structuring, there is a lot we can learn from videos alone. And then, we layer on patient outcome data so we can understand how different surgical techniques/tools/approaches impact the recover of a patient. Stay tuned for what’s next.