De-Identification in Surgical Video: What You Need to Know
As recording surgical procedures quickly becomes the standard of care in the field, maintaining patient and staff privacy within recordings is an issue that all institutions should carefully consider to ensure regulatory compliance and ethical practices.
For video footage, maintaining privacy means de-identifying those who are recorded. If you’re wondering what this involves and how to make sure your institution follows best practices, we’ve got you covered.
What is De-Identification?
The concept of data de-identification arose with the implementation of the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule. The Privacy Rule considers individually identifiable health information to be protected health information. This includes information such as names, birthdates, or social security numbers that are attached to health information, including electronic health information such as recorded surgical videos.
The HIPAA Privacy Rule contains a de-identification standard, which states that health information is considered de-identified if 18 types of identifiers are removed. These include items such as names, dates, medical record numbers, biometric identifiers such as finger and voice prints, and most importantly for video recordings, full-face photographs and any comparable images.
How To De-Identify Surgical Video
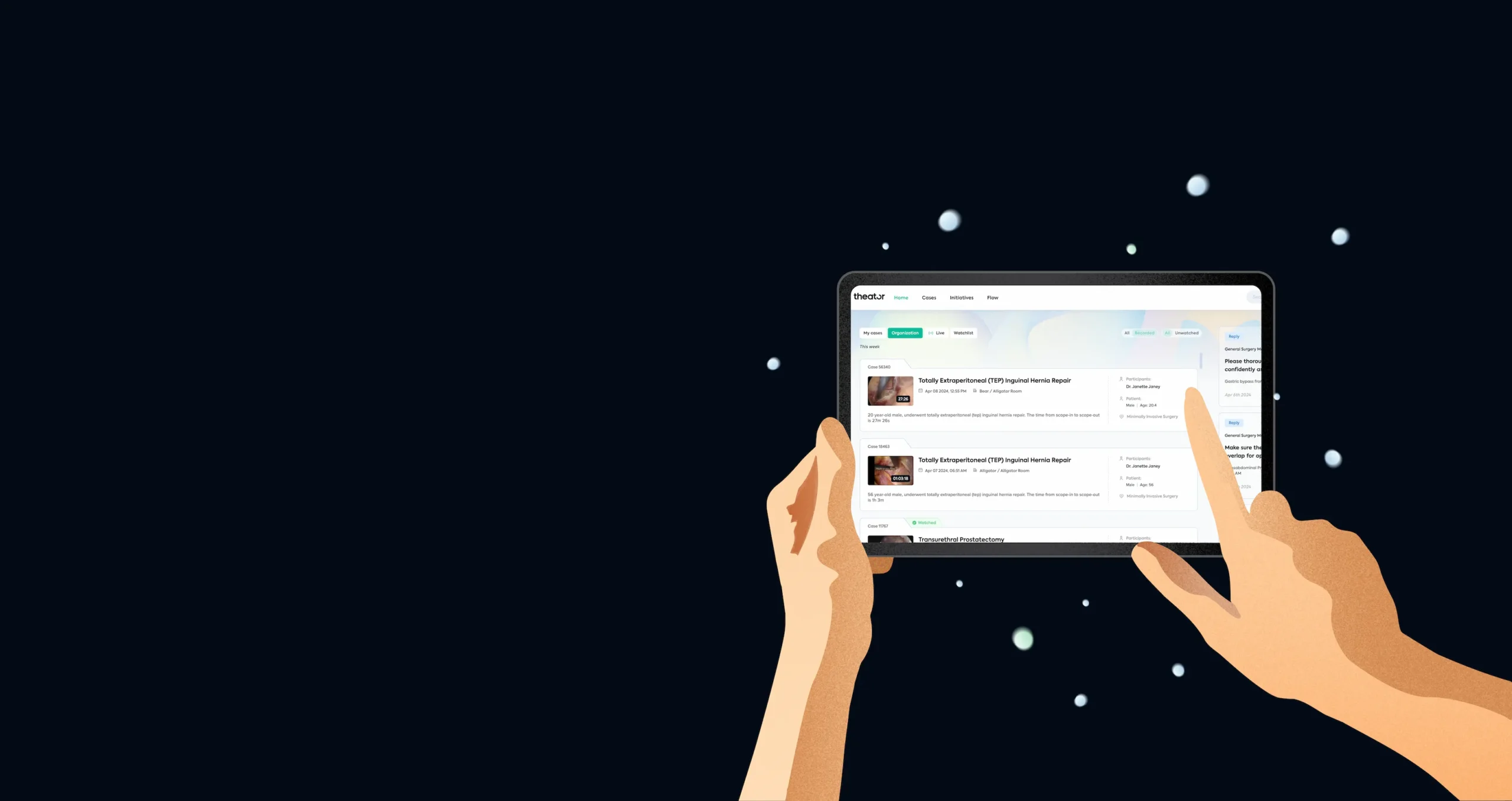
Although it may sound daunting to de-identify an entire surgical video, there are important points to keep in mind that can make the process simple and automated. This was outlined in a recent JAMA Surgery article, in which the Mayo Clinic, in partnership with Theator, set the standard for use, analysis, and de-identification of intracorporeal surgical videos:
1. Obtain consent
Even though obtaining signed consent prior to a surgical procedure is second nature, in the age of recording surgical video it’s important to make sure this process is specifically covered in your surgical consent. Patients should be made aware that their procedure will be recorded, assured that their privacy is protected, and informed about how the recorded footage will be used. Although obtaining consent does not actually de-identify surgical video, it’s a critical first step to ensuring ethical and compliant practices.
2. Remove identifying information
While it may seem like a good idea to include information such as a procedure date or patient medical record number on a recorded video, since these are considered identifiers, it’s best not to do so. This reduces the risk of a surgical video being traced to a specific patient if it is used for educational or other purposes.
3. Automate removal of out-of-body frames
Luckily, the technology already exists to automatically remove out-of-body video footage, which poses the highest risk for identification. By identifying out-of-body video with greater than 99% accuracy, Theator’s surgical platform technology significantly reduces the risk of accidentally including images of patients or staff that could result in identification of protected health information. Automation of this process is the key to success in de-identification, as manual removal of identifying footage would be prohibitively time consuming.
De-Identification in Surgical Video
Although it’s valid to be concerned about the privacy of recorded surgical video, it’s important to know that solutions already exist to overcome the challenges of maintaining patient and staff privacy. By initiating updated consent processes, removing identifiers from recorded material, and implementing a system that automatically identifies and removes out-of-body frames, institutions can meet their patient’s needs for privacy and remain compliant with regulatory standards.