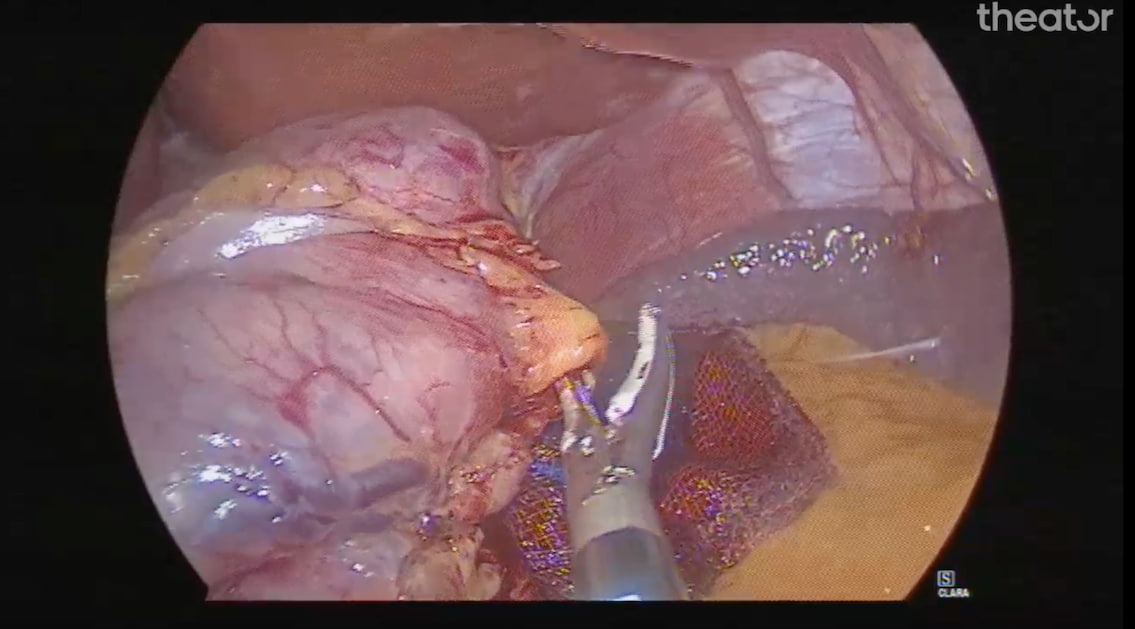
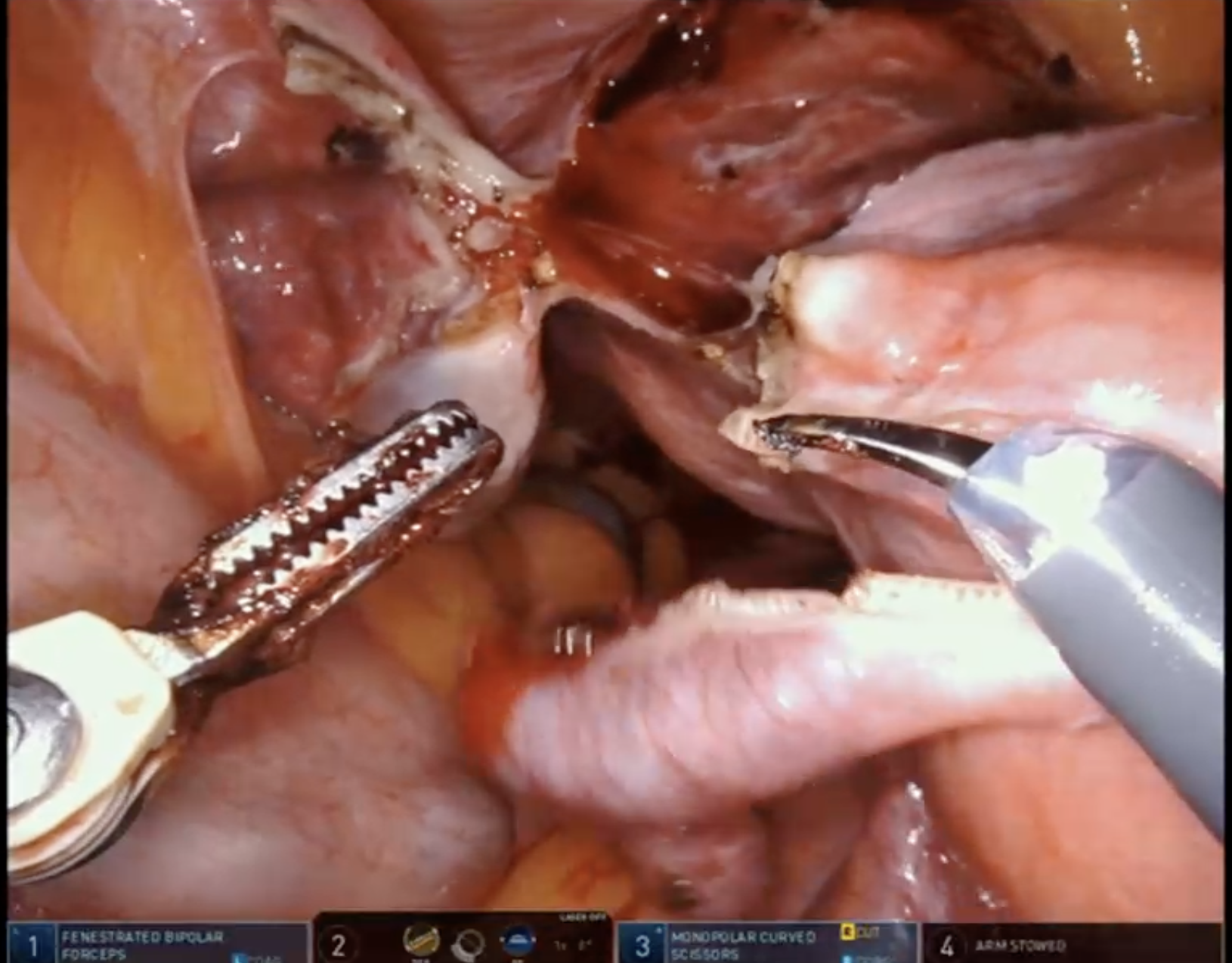
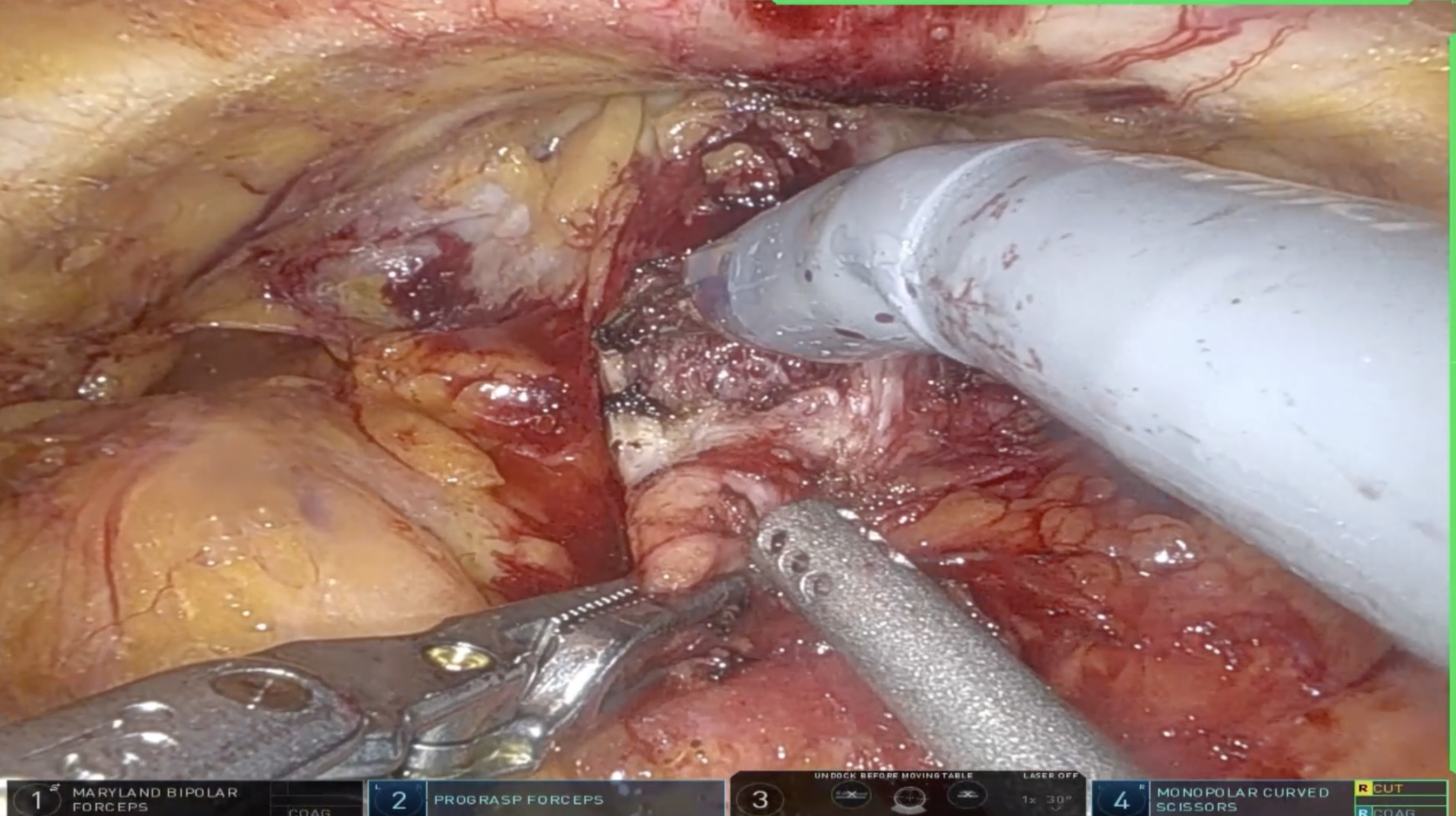
From smart home devices to self-driving cars, AI has become an integral part of our daily lives. That includes healthcare, where AI regularly assists in disease detection, patient monitoring, medical imaging analysis, and more. And now, thanks to advancements in computer vision and machine learning, it’s also making its way into the operating room.
In fact, these days, it seems everyone is talking about how AI can address unmet needs in the OR. Health tech companies large and small are busy developing AI applications intended to improve surgical care. So whether you’re looking to boost team efficiency, streamline inventory management, or identify surgical best practices, you’ll likely have plenty of AI-assisted options to choose from.
But before implementing any new AI tech in your hospital’s ORs, there are a few key considerations you should bear in mind. After all, evaluating AI-based solutions requires a very different set of criteria than, say, trying out the latest surgical stapler.
So, without further ado, here are the top 10 things to look for when evaluating AI technology for the OR, courtesy of our surgical AI and computer vision experts (download the quick reference checklist here):
- Value: First and foremost, the benefits of the technology should outweigh any risks, costs, or drawbacks. Many hospital administrators may be drawn in by the promise of “advanced capabilities” and the “cool factor” of a shiny new AI solution — without realizing it doesn’t actually solve any existing problems or create new opportunities.
- Objectivity: AI is trained on examples of whatever information it needs to analyze or generate. If those examples are biased (based on gender or ethnicity, for example), its output will be biased as well. Particularly in healthcare, AI solutions must deliver objective results to avoid perpetuating — and to eventually eliminate — the bias that already exists in the system.
- Quality Control: AI and computer vision technology for the operating room should feature built-in quality control measures to ensure that only accurate, reliable results are generated. Hospitals should also require regular maintenance and upgrades to keep up with evolving surgical best practices.
- Scalability: As your hospital’s volume of both procedures and procedure types increases, any AI solution must be able to accommodate that growth. That means it should be built for quick, easy implementation across additional ORs, and to some extent, its capabilities should be specialty-agnostic. This is necessary to ensure consistent care for all patients — and a consistent experience for all users.
- Security & Compliance: Any AI technology must maintain compliance with best-in-class security standards in the healthcare industry (e.g. HITRUST certification for software solutions). This includes ensuring that all data generated is de-identified, securely stored, and shareable only with authorization from patients and healthcare providers.
- Interoperability: The last thing you want is AI that creates more work for already-overburdened clinicians and IT admins. Hospitals should choose solutions that integrate seamlessly with existing (and evolving) IT infrastructure, as well as any other systems needed for accessing or managing the data.
- Data Ownership: AI continuously improves as more data is collected and processed — so it’s important to consider both who owns and who ultimately benefits from all that data. Your hospital should retain ownership of its data, while still being able to integrate with and benefit from benchmarking against global datasets in accordance with privacy policies for all entities.
- Effortless Integration: An effective AI solution should automate and/or augment performance of important tasks without interrupting existing workflows. The more training or new steps required to adopt the system, the less likely teams will be to use or get any value from it.
- Explainability: Even if an AI model appears to provide accurate results, those using the solution should be able to understand the rationale behind those results. If no one can explain how the AI works, there’s no way to truly gauge or confirm accuracy, objectivity, or other critical factors.
- Financial Impact: Hospital executives must assess whether an AI tech is cost effective for their institutions. That means its total cost of ownership should be low enough to avoid budget strain. In fact, ideally, the solution should have a net positive financial impact by empowering clinical and administrative teams to do higher volumes of higher quality work in less time and giving patients and prospective surgical staff another reason to choose your hospital over others.
In short, AI has the power to transform surgery, just as it has transformed so many other aspects of modern society. If hospital administrators are discerning about which solutions they adopt and how those solutions are implemented, they can empower surgeons, clinical leaders, and administrators to reach new heights in both operational efficiency and patient care.
Share this story
Ready to start evaluating AI technology for your ORs?
Fill out the form, and we’ll send you a simple checklist summarizing these considerations.

Thank you!
Check your email soon for a link to download the checklist.